July 1, 2010 (Vol. 30, No. 13)
New Tools Seek to Enhance Assessment of Crucial Part of Cell-Based Assays
For obvious reasons, cell viability is an important part of any cell-based assay. That’s why researchers worldwide often try to include some measurement of cell viability in their assay design schema. Like everything in biotechnology, there are many ways to measure cell viability, some of which were presented at the recent annual conferences of the Society for Biomolecular Sciences (SBS) and the American Association of Immunologists (AAI).
For example, Sarah Roberts-Thomson, Ph.D., assistant professor at The University of Queensland, uses MTS cell viability assays to assess the functional consequences of inhibition and overexpression of specific calcium transporters in cancer cell lines.
“Our work is all about identifying and characterizing novel therapeutic targets for cancer, specifically breast and colon cancer,” she said. Her group presented data at the SBS meeting showing the use of these assays to assess the consequences of overexpression of a calcium-permeable ion channel on the viability of a breast cancer cell line.
“Cell viability measurement is a common application of flow cytometry,” said Maria Dinkelmann, Ph.D., lab manager at Accuri Cytometers. “Rather than using more traditional methods, which can be more laborious and less precise, individual researchers that have access to flow cytometry can better measure cell viability either on its own or in conjunction with another biomarker.”
One of the most common traditional techniques used to determine cell viability is the hemocytometer, which is basically a grid that is etched into a metal microscope slide. The typical method calls for the use of Trypan Blue, which is taken up by dead cells but not by viable cells. After mixing their sample with the dye and then applying this mixture to the hemocytometer slide, a researcher will literally count the cells by eye using a light microscope and compare the number of cells that have taken up the dye to the number that have not taken up the dye.
“Hemocytometry is a common technique in a lot of labs and while it has the advantage of accessibility, it also has disadvantages,” said Dr. Dinkelmann. She pointed out that the method is subjective, which results in low precision. It is also a time-consuming and labor-intensive method because of all the manual counting involved.
In contrast, flow cytometry is automated, significantly more objective, and enables the researcher to analyze cell viability in multiple cell populations simultaneously. “However, advanced techniques such as flow cytometry have not been more universally adopted for viability assays because they can be complex to use, expensive, and often require access to core facility systems.”
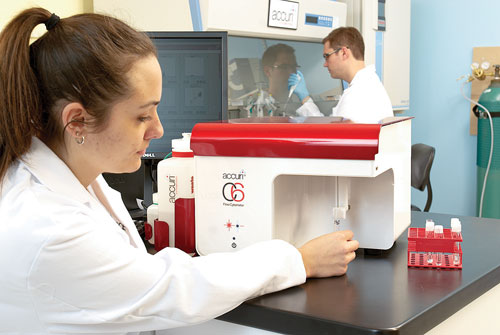
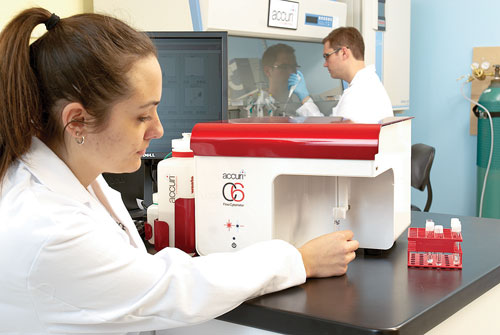
According to Accuri Cytometers, its C6 flow cytometer can be used to measure cell viability less laboriously and more precisely than traditional methods.
At the AAI immunology conference, Dr. Dinkelmann talked about the Accuri C6 Flow Cytometer. The Accuri C6 was explicitly designed to be routinely accessible to individual scientists in their research labs, she noted, combining ease-of-use and affordability along with strong performance. “While we do not have precise data on how our customers are using their C6 Flow Cytometers, anecdotal feedback indicates that measuring cell viability is a common application.”
The beauty of flow cytometry is that it “can measure six or more different parameters and one of those can be cell viability,” said Tom Duensing, Ph.D., vp of product development at IntelliCyt.
Dr. Duensing’s presentation at the SBS conference highlighted HyperCyt, the company’s high-throughput flow cytometry platform. This cell-based screening platform uses flow cytometry as its detection module. In his presentation, Dr. Duensing focused on the instrument’s ability to determine the amount of antibody produced per cell in a test well.
“Antibody-based therapeutics are the largest growing biologic therapeutic modality and developers need to find cell lines that will produce antibodies for them in large quantities. With our technology we can simultaneously measure the amount of antibody that is being produced and secreted into the supernatant in each well, enumerate the number of cells that are in that well, and determine the percentage cell viability in that well.”
The inner workings of their cell viability assay are pretty straightforward. “We add a fluorescent dye that only enters dead or dying cells. When cells that have taken up the dye pass through the laser detection system, they emit fluorescent light that can be measured, allowing us to determine the percentage of cells that are not viable.”
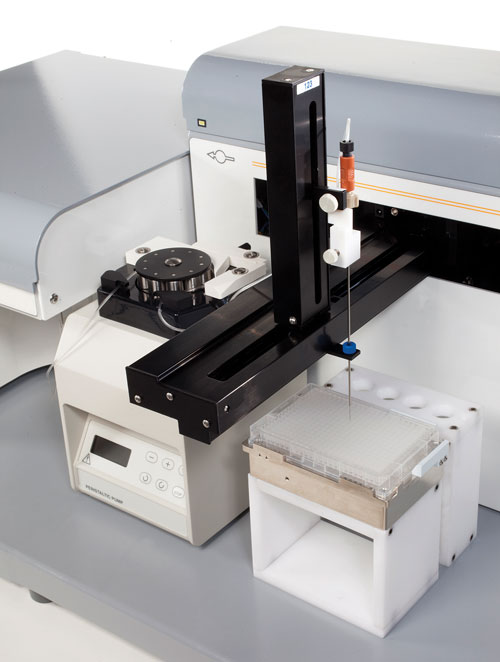
IntelliCyt recently introduced the HTFC Screening System, which bundles the firm’s HyperCyt technology and flow cytometer. It is reportedly amenable to performing high-throughput screens that measure viability in suspension cell cultures as opposed to current technologies that use adherent cells.
Drug Tox Testing
Testing for CYP450 induction is part of drug-drug interaction (DDI) studies, and cell viability assays serve as a control in such studies. Cytochrome P450s are a class of enzymes that catalyze metabolism of drugs, but only a small number of these enzymes catalyze the majority of drug metabolism. Some CYP450 genes are induced by drug compounds. For example, CYP3A4 and -1A2 are important to the FDA because they metabolize a substantial number of drugs and represent two distinct induction pathways.
CYP450 gene inductions are important because they can cause adverse drug-drug interactions. In other words, if two drugs are co-administered and one drug causes the accelerated metabolism of the second one by way of P450 induction, reduced efficacy of the second drug is the result.
Recently, Promega, BioTek Instruments, and Celsis In Vitro Technologies collaborated to produce a multifunctional assay for the measurement of CYP450 induction. “Our assay design lends itself to high-throughput screening,” said Timothy Moeller, scientific advisor at Celsis, who added that an important novelty of the collaborative assay design is that these assays have not previously been performed in 384-well plates.
“As DDI studies are moved into a 384-well format, and a greater number of compounds are evaluated, it is essential to incorporate automation into the assay process,” said Brad Larson, principal scientist at BioTek. Two instruments from BioTek were used in the new design to handle all liquid handling functions.
“Each liquid handler has a small footprint enabling it to be placed into existing laminar flow hoods. Due to the fact that induction assays are typically performed over multiple days, sample sterility is extremely important. Automation such as that used here allows the researcher to greatly reduce or eliminate the risk of contamination without having to exhaust the monetary resources of the research lab,” added Larson.
Celsis supplied the human hepatocytes that are the third component of this collaborative assay design effort. Hepatocytes give all the individual variation of real liver cells including variable induction of cytochrome P450s, making them the gold standard for this cell-based tox testing. “Toxicity in cell culture is well established as a predictor of toxicity in the whole animal or human being,” said James Cali, Ph.D., R&D director, assay design at Promega.
The cell viability and CYP3A4 assay technologies are Promega’s CellTiterGlo and P450-Glo, respectively. “Our CellTiterGlo product correlates ATP level to cell viability.” The CYP3A4/1A2 multiplex relies on the combined strength of a luminescent substrate for CYP3A4 and a fluorescent one for CYP1A2. The addition of the CellTiterGlo viability assay adds a parameter for normalization to cell number and simultaneous toxicity testing.
“Our assay configuration was designed for discovery-phase ADME testing. This method allows the drug company to characterize multiple compounds for DDI and toxicity liabilities so as to fail problematic compounds early and cheap.” Dr. Cali added that by increasing throughput, adding automation, and reducing well volume, drug companies are able to apply what has traditionally been late-stage analysis to an early secondary profiling stage.