Researchers at the University of Bonn and the University of Singapore have discovered a new intracellular “smoke detector.” The intracellular sensor detects damage to the mitochondria. The sensor may also help lead to novel therapies for unimpaired heart and bowel function.
The findings are published in Nature Immunology in a paper titled, “Mitochondrial damage activates the NLRP10 inflammasome.”
“We have now discovered that a molecule called NLRP10 also acts as a sensor,” explained Eicke Latz, MD, PhD, head of the Institute of Innate Immunity at the University Hospital Bonn. “This was completely unknown until now.”
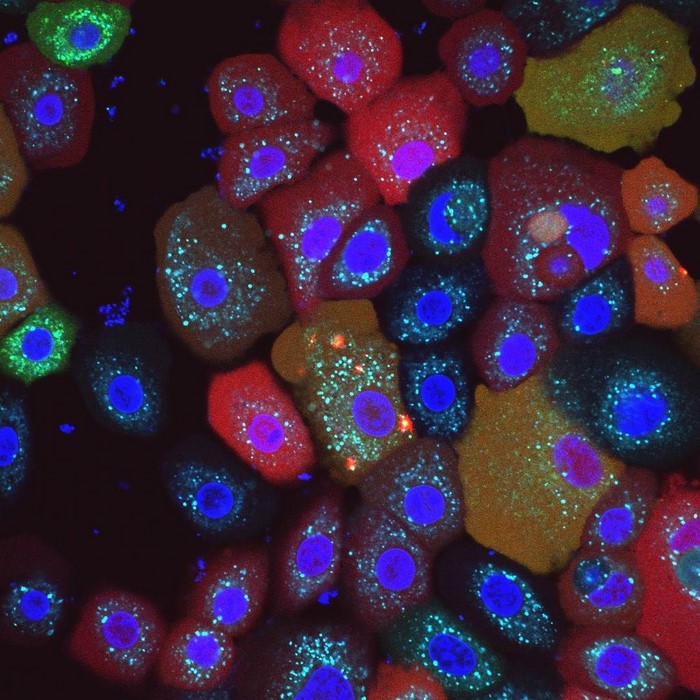
“Upon detecting pathogens or cell stress, several NOD-like receptors (NLRs) form inflammasome complexes with the adapter ASC and caspase-1, inducing gasdermin D (GSDMD)-dependent cell death and maturation and release of IL-1β and IL-18,” wrote the researchers. “The triggers and activation mechanisms of several inflammasome-forming sensors are not well understood. Here we show that mitochondrial damage activates the NLRP10 inflammasome, leading to ASC speck formation and caspase-1-dependent cytokine release.”
Figuratively speaking, NLRP10 detects when the mitochondria in the cell start to smoke due to some malfunction. As soon as an NLRP10 sensor detects damage to mitochondria, it creates a so-called inflammasome, a complex molecular machine. Its activity ultimately causes the cell to perish and be disposed of by summoned immune cells.
“This process is hugely important,” explained Latz, who is also the spokesperson for the Cluster of Excellence ImmunoSensation2 and a member of the Transdisciplinary Research Area “Life and Health” at the University of Bonn. This is because the inflammasome ensures that the fire is stamped out straight away, which prevents a prolonged smoldering fire that would damage other parts of the tissue. “Disruption of this mechanism can result in chronic inflammation,” the researcher emphasized. “Killing cells with mitochondrial defects may sound drastic. Ultimately, however, this step prevents more serious consequences.”
“If a mutation causes the NLRP10 sensor to malfunction, this can result in a chronic skin inflammation called atopic dermatitis,” explained Tomasz Próchnicki, who performed an important part of the experiments for his doctorate in Latz’s research group.
Large quantities of NLRP10 are also found in the intestinal wall cells. These also have regular contact with pathogens and potentially harmful substances. Another organ in which the sensor can be detected is the heart: It is particularly dependent on a well-functioning energy supply. This may make it especially important to quickly kill and replace cells with defective mitochondria.
The study may potentially also open up new therapeutic perspectives. “It is conceivable to specifically modulate the NLRP10 sensor using certain substances in order to stimulate the formation of inflammasomes,” Latz explained. “This approach might enable chronic skin diseases to be better controlled.”