DNA-based gene therapy, the usual kind of gene therapy, is hard to deliver compared to RNA-based gene therapy. New DNA must enter the nucleus after being transported by nanoparticles or viral vectors, which can be inefficient or immunogenic. But once new DNA is in place, it has the advantage of being controllable. Gene expression may be turned up or down by any of several well-established methods. This kind of control has been lacking for RNA-based gene therapy, even though RNA promises safer, easier delivery.
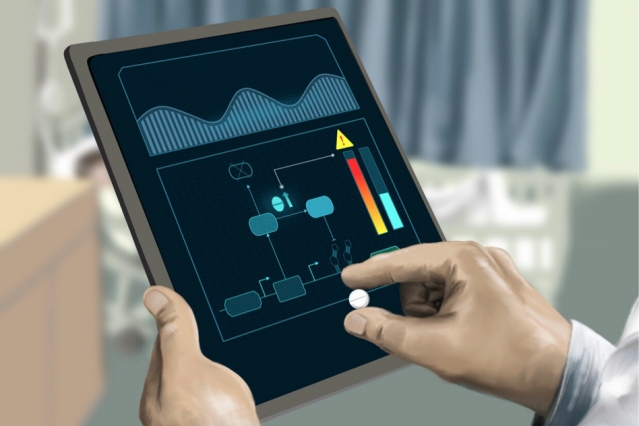
A new study suggests that RNA-based gene therapy may become more controllable through the introduction of RNA circuits. According to this study, which comes from scientists based at MIT, RNA transcripts that encode for therapeutic proteins can be delivered along with RNA transcripts that encode for RNA-binding proteins. These RNA-binding proteins can be designed to respond to small-molecule drugs and favor or disfavor, as needed, the expression of the protein-encoding RNA transcripts.
Details of the new approach to RNA-based gene therapy appeared October 16 in the journal Nature Chemical Biology, in an article titled, “Small-molecule-based regulation of RNA-delivered circuits in mammalian cells.” The article describes a platform for small-molecule-based regulation of expression from modified RNA (modRNA) and self-replicating RNA (replicon) delivered to mammalian cells.
“We engineer small-molecule-responsive RNA binding proteins to control expression of proteins from RNA-encoded genetic circuits,” the article’s authors wrote. “Coupled with specific modRNA dosages or engineered elements from a replicon, including a subgenomic promoter library, we demonstrate the capability to externally regulate the timing and level of protein expression.”
Essentially, these control mechanisms facilitate the construction of ON and OFF switches. In addition, combinations of ON and OFF switches can yield two-output switches, which support the use of inducers for choosing between one of two gene expression states. Such switches could allow doctors to more accurately tailor treatments for individual patients. They also offer a way to quickly turn gene transcripts off, if necessary.
“Due to the dynamic nature of replication, the circuits' performance can be tuned to allow different proteins to express at different times, all from the same strand of RNA,” says Jacob Becraft, an MIT graduate student and one of the lead authors of the current study.
“Historically, gene therapies have encountered issues regarding safety,” he continues. “But with new advances in synthetic biology, we can create entirely new paradigms of 'smart therapeutics' that actively engage with the patient's own cells to increase efficacy and safety.”
The MIT-led team, which includes the current study’s senior authors, Tasuku Kitada, a former MIT postdoc, and Ron Weiss, an MIT professor of biological engineering, have started a new company, Strand Therapeutics, that is applying the new RNA-based gene therapy approach to cancer immunotherapy.
Using RNA, the researchers plan to develop circuits that can selectively stimulate immune cells to attack tumors, making it possible to target tumor cells that have metastasized to difficult-to-access parts of the body. For example, it has proven difficult to target cancerous cells, such as lung lesions, with mRNA because of the risk of inflaming the lung tissue. Using RNA circuits, the researchers first deliver their therapy to targeted cancer cell types within the lung, and through their genetic circuitry, the RNA would activate T-cells that could treat the cancer's metastases elsewhere in the body.
“The hope is to elicit an immune response which is able to pick up and treat the rest of the metastases throughout the body,” Becraft notes. “If you're able to treat one site of the cancer, then your immune system will take care of the rest, because you've now built an immune response against it.”
Using these kinds of RNA circuits, doctors would be able to adjust dosages based on how the patient is responding, the researchers say. The circuits also provide a quick way to turn off therapeutic protein production in cases where the patient's immune system becomes overstimulated, which can be potentially fatal.
In the future, the researchers hope to develop more complex circuits that could be both diagnostic and therapeutic—first detecting a problem, such as a tumor, and then producing the appropriate drug.