Obesity can promote the spread of breast cancer by inhibiting a metabolic enzyme, acetyl-coenzyme A-carboxylase 1 (ACC1), a central component of fatty acid synthesis. The inhibition of ACC1, report scientists based at Helmholtz Zentrum München, triggers a series of molecular events that culminates in the induction of metastasis.
The scientists also say that blocking this inhibition, via a receptor-blocking antibody, reduced the spread of breast cancer in an experimental model. Such interventions, the scientists suggest, represent a “metabolocentric” approach, one that could add to treatment options for preventing breast cancer metastasis and recurrence
Details of the scientists’ work appeared October 19 in the journal Cell Metabolism, in an article entitled “Acetyl-CoA Carboxylase 1-Dependent Protein Acetylation Controls Breast Cancer Metastasis and Recurrence.” The article noted that ACC1 phosphorylation was increased in invading cells both in murine and human breast cancer, serving as a point of convergence for leptin and transforming growth factor-β (TGFβ) signaling.
“ACC1 is a key component of fatty acid synthesis,” said Mauricio Berriel Diaz, Ph.D., a senior author of the current study and deputy director of the Institute for Diabetes and Cancer (IDC) at Helmholtz Zentrum München. “However, its function is impaired by the cytokines leptin and TGFβ.” The levels of these cytokines are increased particularly in the blood of severely overweight subjects.
The number of people with obesity is increasing rapidly worldwide. The German Cancer Research Center (DKFZ) recently reported that according to the World Health Organization (WHO) the number of children and adolescents with obesity increased tenfold between 1975 and 2016. Besides inducing cardiovascular diseases and other diseases, obesity also promotes the development of cancer and metastases.
Although obesity has been known to be associated with the enhanced spread of cancer, the underlying mechanisms have often remained obscure. One mechanism, however, has been delineated in the current study.
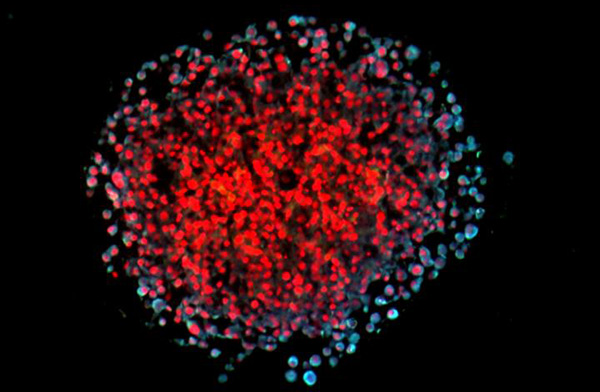
“ACC1 phosphorylation was mediated by TGFβ-activated kinase (TAK) 1, and ACC1 inhibition was indispensable for the elevation of cellular acetyl-CoA, the subsequent increase in Smad2 transcription factor acetylation and activation, and ultimately epithelial-mesenchymal transition and metastasis induction,” wrote the authors of the Cell Metabolism article. “ACC1 deficiency worsened tumor recurrence upon primary tumor resection in mice, and ACC1 phosphorylation levels correlated with metastatic potential in breast and lung cancer patients.”
Essentially, the scientists demonstrated that the described inhibition of ACC1 leads to the accumulation of the fatty acid precursor acetyl-CoA. This precursor is transferred to certain gene “switches” that in turn increase the metastatic capacity of cancer cells by activating a specific gene program.
“Using human tissue from breast cancer metastases, we were able to show that ACC1 was significantly less active there,” said Marcos Rios Garcia, Ph.D., first author of the study. When the scientists blocked the newly uncovered signaling pathway with an antibody (directed against the leptin receptor), this led to a significantly reduced metastatic spread of breast cancer tumors in an experimental model.
In the future, the researchers want to substantiate the data on the newly discovered mechanism in further studies. In addition, they are also considering related intervention points that could possibly be exploited therapeutically.
“Blocking the signaling pathways and switching off the metastasis-related genes could be a therapeutic target,” noted Stephan Herzig, Ph.D., co-senior author of the article and director of the IDC and professor for Molecular Metabolic Control at Technische Universität München and Heidelberg University Hospital. “As part of the so-called neoadjuvant therapy, the risk of metastases or the recurrence of tumors could be reduced prior to the surgical removal of the tumor.”