Scientists in Dallas have identified three drug molecules that reverse resistance to chemotherapy in cultures of aggressive, multidrug-resistant (MDR) forms of ovarian, prostate, and breast cancer. The molecules, originally discovered using high-performance supercomputing, act by blocking P-glycoprotein (P-gp), a transmembrane pump that prevents chemotherapy drugs from accumulating in and killing cancer cells. Reporting in Scientific Reports, the South Methodist University (SMU) team, led by Pia Vogel, Ph.D., and John G. Wise, Ph.D., suggest that the P-gp inhibitors “may be promising leads for future drug development.” Their published paper is entitled “Targeted Inhibitors of P-Glycoprotein Increase Chemotherapeutic-Induced Mortality of Multidrug-Resistant Tumor Cells.”
MDR remains a major obstacle to the effective treatment of many adult and pediatric cancers, the researchers write. A primary mechanism of drug resistance in cancer cells is overexpression of drug efflux transporters, including one of the most well studied, P-gp, overexpression of which renders many different types of cancer resistant to chemotherapy.
Transmembrane pumps are expressed by healthy as well as cancer cells and act to clear the cells of toxins. Some cancers ramp up expression of pumps such as P-gp, and another pump known as breast cancer resistance protein (BCRP), in response to anticancer drug therapy. “The cancer cell itself can use all these built-in defenses to protect it from the kinds of things we're using to try to kill it with,” says Wise,” who is associate professor in the SMU Department of Biological Sciences. “If enough of the pumps are present, the cancer isn't treatable anymore.”
Pumps such as P-gp and BCRP may not initially be present in cancer cells at high levels, but after a first round of chemotherapy, surviving cancer cells can bump up production of the proteins. Subsequent rounds of chemotherapy are then far less effective because the chemotherapeutic agents can't accumulate in the cells.
The compounds developed by the SMU team were not themselves effective against cancer, but by blocking the overexpressed P-gp drug pumps, they allowed chemotherapy to build up in and kill the cancer cells. Two of the identified compounds were specific to P-gp, and the third also blocked the BCRP pump, although to a lesser extent.
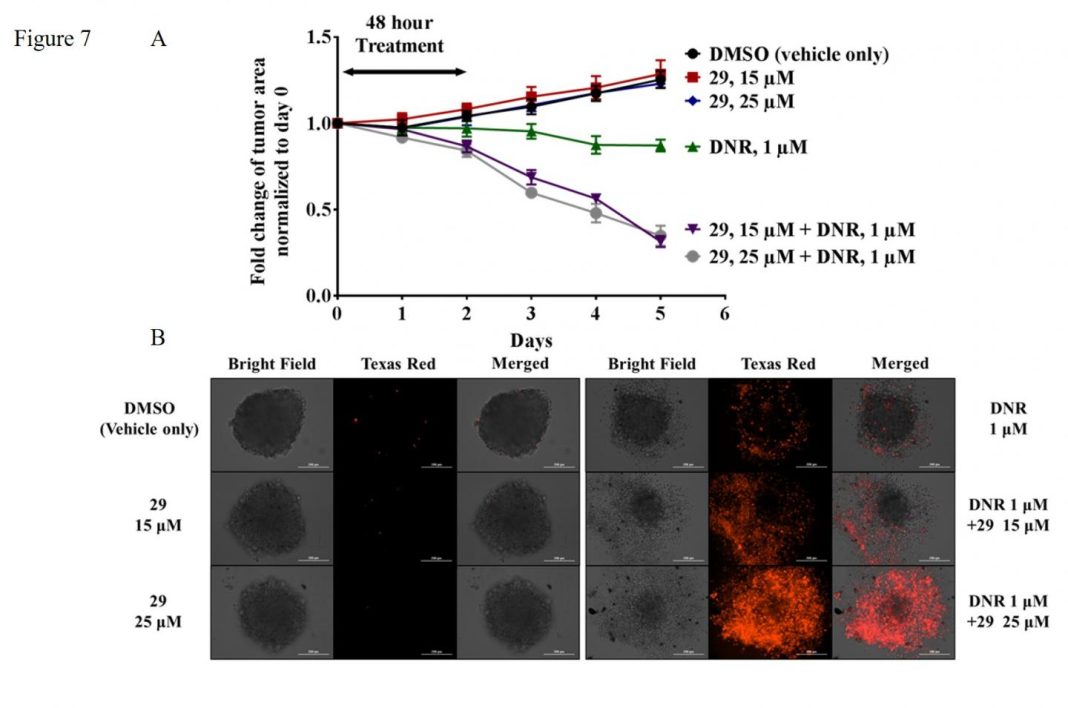
The team tested the three P-gp inhibitors in combination with chemotherapy in 2D cultures of chemotherapy-resistant ovarian and prostate cancer cell lines and 3D microtumor prostate cancer cultures. The results confirmed that the P-gp inhibitors increased chemotherapeutic accumulation in the cells, reduced cell viability and colony formation, inhibited cell migration, and increased cell death. “They effectively bring the cancer cells back to a sensitivity as if they'd never seen chemotherapy before,” notes Vogel, a professor and director of SMU's Center for Drug Discovery, Design and Delivery. “And our data indicated the molecules aren't cancer specific. They can be used to treat all kinds of cancers because they inhibit not just the P-gp pump, but also the breast cancer protein pump.”
“We wanted to make sure when using these really aggressive cancers that if we do knock out the pump, that the chemotherapy goes in there and causes the cell to die, so it doesn't just stop it temporarily,” Wise adds. “We spent a fair amount of time proving that point. It turns out that when a cell dies it goes through very predictable morphological changes. The DNA gets chopped up into small pieces, and we can see that, and so the nucleus becomes fragmented, and we can see that. Under the microscope, with proper staining, you can actually see that these highly drug-resistant prostate cancer cells, for example, are dead.”
The SMU team acknowledges that P-gp inhibitors already in development have shown “limited success in the clinic.…Unfortunately, to date none of the P-gp inhibitors previously identified and pursued as potential co-therapeutics for treatment of MDR diseases has been successful in clinical trials.” They note that the most recent trials with the P-gp inhibitor tariquidar demonstrated toxicities, “and several Phase III trials have been abandoned.…” A Phase III study with another P-gp inhibitor zosuquidar, was completed, but didn’t show benefits in the older acute myeloid leukemia patient cohort.” Nevertheless, the researchers stress, “despite limited success in the clinic, P-gp still seems an important and relevant target for drug discovery and development.”
Many of the pump inhibitors developed previously are thought to attach to the drug-binding domains of the proteins and stop them from exporting chemotherapeutics by themselves functioning as P-gp transport substrates, and so compete for transport cycles. In contrast, the SMU team’s studies suggest that the three P-gp inhibitors are not themselves P-gp transport substrates, nor do they cause downregulation of P-gp expression in the cancer cells. Their computational studies took into account detailed 3D models of P-gp to identify candidates that had the potential to overcome problems associated with previous P-gp inhibitors, by specifically interacting with the nucleotide-binding domains of the pump and not to the drug-binding domains.
P-gp has been a target for drug discovery for almost 40 years, the researchers note. And while other investigators have described P-gp inhibitors that interact with the nucleotide-binding domains of P-gp, none of these has yet reached the clinic. Others researchers have also recently reported in silico drug discovery studies, the team adds. “However, these studies targeted the drug-binding domains in attempts to disrupt drug transport by P-gp. This approach may lead to P-gp inhibitors that are transported by P-gp, a characteristic that we have tried to avoid.”
“Nature designs all cells with survival mechanisms, and cancer cells are no exception,” Vogel comments. “So it was incredibly gratifying that we were able to identify molecules that can inhibit that mechanism in the cancer cells, thereby bolstering the effectiveness of chemotherapeutic drugs. We saw the drugs penetrate these resistant cancer cells and allow chemotherapy to destroy them. While this is far from being a developed drug that will be available on the market anytime soon, this success in the lab gives us hope for developing new drugs to fight cancer.”