Helen Albert Writer GEN
Using Multi-Omic Technology to Reclassify and Improve Treatment for Autoimmune Disease
Despite the large number of people affected by these chronic conditions, many remain undertreated and underdiagnosed. No cure for autoimmunity has been found, and the cause of many such diseases is still unknown.
The complexity and heterogeneity of many autoimmune diseases has previously made them hard to define and treat. However, the recent rapid rise of omics technologies has facilitated a new approach to the study of these conditions.
“The multi-omic approach has the potential to unveil novel aspects of disease pathology as well as identify multiple biomarkers, that then can be targeted for therapeutic intervention as well as monitoring responses to such interventions,” Fozia Mir, Ph.D., Tisch MS Research Center of New York, explained.
While scientists acknowledge that research into more effective treatments for autoimmune disease still lag fields such as cancer, progress toward better diagnosis, monitoring, and treatment is slowly being made. With the aid of new and rapidly advancing technology, there may yet be light on the horizon for the many thousands of patients with these chronic, often debilitating conditions.
A Technological Revolution
Many gene-association studies in patients with autoimmune disease were carried out following the sequencing of the human genome. Although many genetic associations were observed, they were difficult to replicate across patient cohorts and did not take environmental influences into account.
“We realized that what is important is not the specific gene involved in that specific disease, rather what the gene does, what function it controls,” said Alessio Fasano, M.D., division chief, pediatric gastroenterology and nutrition; and director, Center for Celiac Research and Treatment at Massachusetts General Hospital.
Using transcriptomics, or RNA sequencing, scientists can study gene expression in a sample from a patient at a given time, or to monitor change in gene expression over time from multiple samples. This has clear advantages for research into autoimmune disease (see sidebar).
Proteomics is also being widely used in autoimmune research to analyze molecules secreted by a variety of immune cells including autoantibodies and cytokines.
This is a focus for Paul Utz, M.D., professor of immunology and rheumatology, Stanford University School of Medicine, and his team. They are using bead-based multiplex arrays, which allow investigation of around 250 analytes simultaneously, to better diagnose, subset, and treat patients with these conditions.
“Once you know if patients are in a particular subset that might be at greater risk of various clinical phenotypes or clinical signs or symptoms, then you can customize therapy based on the results,” he explained.
Utz and his team are also looking at how a person’s epigenome could influence their immune system. They found a significant epigenetic difference between the immune system of elderly versus young individuals and are doing comparisons with patients with autoimmune disease.
Our hypothesis is that as we look at immune cells derived from people with autoimmune diseases that they are going to look more like old people with a defective immune system than otherwise healthy young people,” Utz said.
When asked what technological advancements he considered particularly significant over the last few years, Utz highlighted single-cell RNA sequencing and its ability to identify completely new cell types. He also praised a method used in molecular biology to study the accessibility of chromatin called ATAC-seq (Assay for Transposase-Accessible Chromatin using sequencing).
“People can see what the genetic regulators are, what transcription factors are driving the process, what part of the chromatin is open and how it changes in disease or following therapy,” he explained. “Then CyTOF (mass cytometry) has really revolutionized how we can look at about 40 different cell markers at a time.”
Metabolomics, which assesses cellular metabolites using mass spectrometry and high-resolution proton nuclear magnetic resonance, is another omics technology being used to study autoimmune disease.
“We are currently utilizing metabolomic screening of cerebrospinal fluid from multiple sclerosis patients,” commented Mir.
She added: “The metabolome represents the amplified sum total of the changes occurring in a particular state (normal vs. diseased). We hope to identify novel biomarkers of disease activity and progression as well as discover potential therapeutic targets by unraveling the altered metabolome in multiple sclerosis.”
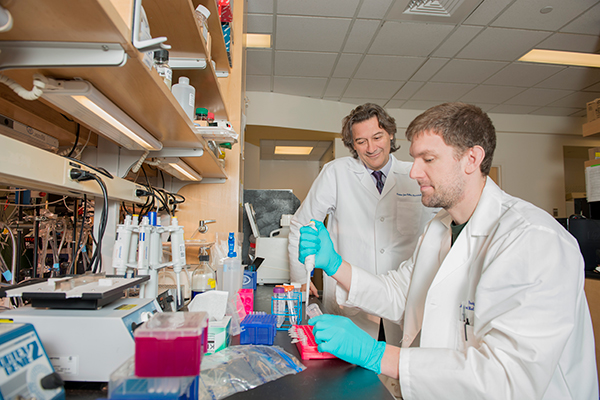
Alessio Fasano, M.D. (l) and researcher in the lab at the Center for Celiac Research and Treatment.
Reclassifying Autoimmune Disease
Marta Alarcón-Riquelme, M.D., Ph.D., University of Granada, Spain, is one of the lead researchers for the PRECISE-SADs project. Its aim is to use multi-omic techniques and bioinformatics to reclassify the six systemic autoimmune diseases represented by the study’s 2871 patients located in 12 different countries.
The researchers hope information gained through this project will allow new biomarkers and drug targets to be identified to help diagnose and treat these patients more effectively.
“This way of reclassifying diseases, it has been done a lot in cancer. We have lung cancer, prostate cancer, breast cancer and so on, but the people working on cancer have been smart enough to use the term ‘cancer’ for all of them. Now we have to say ‘autoimmunity’,” commented Alarcón-Riquelme.
Fasano and his team believe the microbiome may play an important role in the onset of autoimmune disease and are currently recruiting children into the Celiac Disease Genomic Environmental Microbiome and Metabolomic Study (CDGEMM).
The aim of CDGEMM is to follow children who have a first-degree relative with celiac disease, and are therefore at risk themselves, to try to understand what triggers could precipitate the onset of autoimmunity.
As Fasano expanded: “We hope that will give us the subgroups, and possible targets, to stop the chain of events that leads to the autoimmune process, with the outcome being twofold: one, personalized medicine; and two, primary prevention, [to] intercept the disease before it happens.”
Source: NIAID, NIH
In the Clinic
While use of multi-omics techniques to study autoimmune disease is relatively new, and research is largely focused on diagnosis and classification, early findings are already beginning to impact patients.
Utz and his team are using their bead-based array technology to analyze samples from patients with autoimmune disease who are undergoing treatment in clinical trials.
“We are very interested in trying to figure out who a responder or a non-responder might be,” he commented. “If you think about it, the gain to the healthcare system would be enormous. If you could predict that someone was not going to respond to a drug, or to have a bad outcome, then you wouldn’t bother trying give it to them for three months to show that it didn’t work.”
Early research by Fasano and colleagues discovered a protein—zonulin—that appeared to be an early biomarker of type 1 diabetes and celiac disease, as well as being linked to loss of function in the intestine.
There is evidence that gut bacteria could trigger the secretion of this protein. Inhibitors of zonulin are now being tested in clinical trials for celiac disease. Innovate Biopharmaceuticals announced this summer that its zonulin inhibitor, larazotide acetate, was due to enter Phase III clinical trials later this year.
There seems to be a consensus that use of multi-omics techniques can facilitate the move toward a more personalized treatment approach for patients with autoimmune disease.
“Experiencing the era of big data and precision medicine, multi-omics data empowers tailored-made theranostics and thus, patient stratification and optimum disease management,” said Theodora Katsila, Ph.D., a senior research scientist at University of Patras, Greece.
Mir added: “Omic studies not only will further our understanding of disease processes, they also allow for development of multiple biomarkers to assess and monitor drug efficacy and safety. Furthermore, it should be possible to personalize these decisions for each patient objectively.”
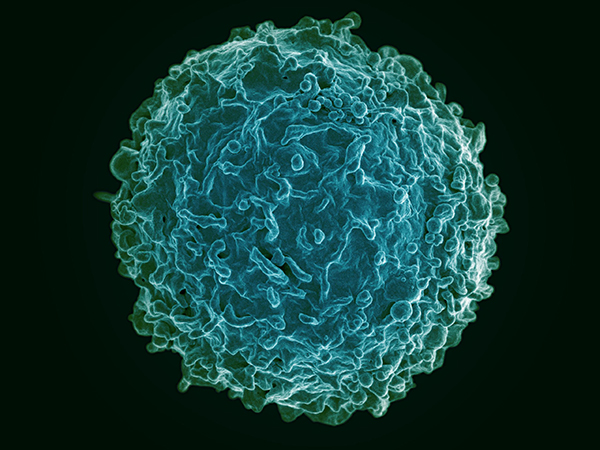
Colorized scanning electron micrograph of a B cell from a human donor. [NIAID, NIH]
Future Directions
Looking into the future, Fasano admitted the current fast pace of technology development makes it hard to predict what will be achievable within the next couple of years. “Of course the goal, the holy grail, is to find biomarkers that can help us to predict who with a specific genetic background may eventually go in the wrong direction and let us bring them back.”
However, he conceded: “a much more obtainable and more near future goal is using these biomarkers for patient stratification so that you can customize better treatments for a specific subgroup of individuals.”
Indeed, this approach is one that a number of groups seem to be adopting, including those of Mir and Alarcón-Riquelme. The latter hopes the approach used in PRECISE-SADS will allow a more accurate reclassification of autoimmune conditions to allow a more personalized and effective approach to treatment.
In addition to the development of companion diagnostics, Utz believes that within the next few years it will be possible to use omics technology to predict which therapies specific patients will respond to, and which they will not.
Potential challenges for the field include the sheer amount of data that is produced using a multi-omic approach. This could make extensive analysis difficult and would rely on concurrent advances in data science research.
Another challenge relates to cost-effectiveness, and ease of use of the technology. Both need to be considered to maximize the chances of any technique or test being used in the clinic or in countries outside the United States and Europe.
“We need to try to see whether we can define better treatments in order to be able to give them something that is useful. Let’s put it like this, not just in Europe, not just in the U.S., all around the globe. Something that is easy to use,” Dr Alarcón-Riquelme concluded.
This article was originally published in the January/February 2018 issue of Clinical OMICs. For more content like this and details on how to get a free subscription, go to www.clinicalomics.com.



