Sponsored content brought to you by
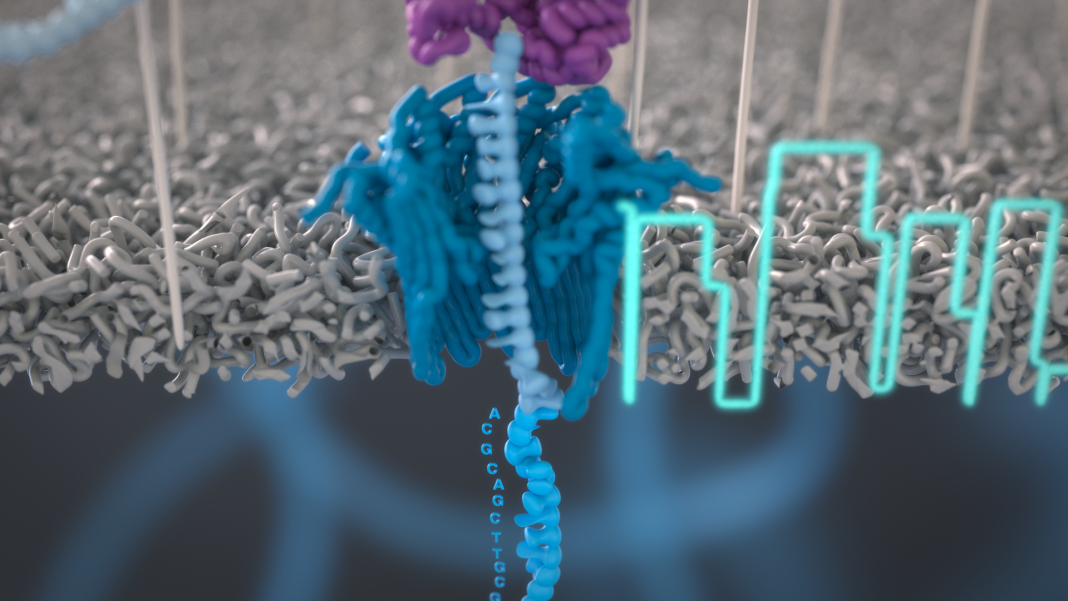
Cervical cancer is caused almost exclusively by the human papilloma virus (HPV) and has a large mortality burden, especially in the developing world. HPV has a 7.9 kb genome and replicates in the nucleus as a circular, extrachromosomal element, termed an episome, by hijacking host cell machinery. It encodes two oncogenes, E6 and E7, which inhibit the host tumour suppressor genes p53 and RB1 respectively. Integration into the genome frequently leads to deletion of viral replication proteins E1 and E2 and contributes to chromosomal instability.
The HPV genome is found integrated in 70% of cervical cancers. Integration events frequently occur near oncogenes, and this is associated with their increased expression. These events can also be quite complex, making them challenging to resolve with short-read sequencing technologies. At London Calling 2022, Vanessa Porter and Michael Dean showcased how long nanopore reads could be used to examine the impact of integration on both the human and HPV genome *.
The complex landscape of HPV integration events
Using PromethIONTM, Vanessa Porter (Canada’s Michael Smith Genome Sciences Centre, Canada) and her team generated whole-genome sequencing data for 66 cervical cancer clinical research samples from Ugandan and USA cohorts. Vanessa developed her own custom pipeline to call HPV integration breakpoints as translocations. Vanessa highlighted how the benefit of long reads is that ‘you can identify integration events that may span multiple chromosomes, or that are linked together from great distances through structural rearrangements’. Across the samples, Vanessa observed integration events that could be classified into one of six categories. Whilst the actual content of the inserted HPV sequence was often variable, E6 and E7 sequences remained constant, suggesting they are a prerequisite for cervical cancer formation.
One of the six integration events involved two breakpoints existing on separate chromosomes and resulted in full chromosome arm translocations, exemplified by chr12 and chr4 sandwiching a piece of HPV DNA. Vanessa noted how ‘this is exactly the type of event that nanopore sequencing allows us to identify, since the reads are able to pass over the HPV, sequencing into the next chromosome.’ Vanessa also examined how the landscape of integration events varies between HPV types. Multi-breakpoint integration events were most frequently observed in HPV16.
Leveraging an ‘additional bonus of nanopore sequencing’, owing to the PCR-free direct detection of DNA, Vanessa sought to analyse how HPV methylation patterns impacted the human genome surrounding the integration event. With long nanopore reads the data could be readily phased into haplotypes. Vanessa observed that the human genome had a sweep of demethylation for large regions upstream of the breakpoint (up to 400 kb), when compared to the unintegrated haplotype. Furthermore, Vanessa explored how HPV methylation patterns were affected by the integration event. The upstream regulatory regions of HPV remained unmethylated, whilst the genic portions were distinctly more methylated when compared to unintegrated episomal HPV, although variability was observed between HPV types.
HPV – pulling the epigenetic strings
Michael Dean (National Cancer Institute, USA) has been using nanopore sequencing to untangle the role of HPV in driving cancer phenotypes. He, too, has used long nanopore reads to delineate complex integration events. Michael is now shifting focus to see how HPV infection impacts genes regulating the epigenome, thereby altering gene expression and driving carcinogenesis. Michael drew comparisons to embryology, and the differentiation of cells into specialised cell lineages: every stem cell contains the same DNA, yet it’s their unlocking of certain epigenetic programs that govern their differentiated fate. Parallels can be drawn in cancer cells; for example, if a cancer cell needs more oxygen, it can alter the epigenome to turn on angiogenesis pathways. The question that Michael asked was: how are these genes that alter the epigenome impacted by HPV?
To begin to answer this question, Michael used the MinIONTM device – or as he referred to it, ‘this little beast’ – which is the same size as a Swiss army knife he had growing up. He started out by performing full-length cDNA sequencing on 20 HPV+ cancer cell lines and gained ‘unprecedented detail’ on the expression of HPV. In the CaSki cell line, in which hundreds of copies of HPV are integrated into the human genome, only one copy of HPV was expressed; the rest were silent. Furthermore, of the 20 or so isoforms that HPV can produce, the most predominant transcript was an isoform of the E7 oncogene. Similar observations were made in the Snu1000 cell line, containing many copies of episomal HPV. Michael described how the virus is therefore ‘regulating its epigenome in order to express the oncogene it needs later in life.’ HPV integration was found to upregulate genes near the site of integration, some of which were oncogenes that Michael surmised ‘were probably playing some role in the transformation process’. Michael also turned to direct RNA nanopore sequencing, whereby native RNA molecules are sequenced, hence avoiding reverse transcription bias and enabling RNA modification calling. He applied this method to HeLa cell lines, in which HPV integrated near the MYC oncogene, where significant MYC overexpression was observed. Michael shared how his PhD had focused on studying MYC expression; he highlighted how he ‘never imagined that …[he] would directly see RNA transcripts’.
Like Vanessa, Michael explored how methylation was affected by HPV integration. He benchmarked his results against short-read bisulfite sequencing and found that ‘nanopore sequencing gave highly accurate methylation calls’, stating that the ‘beauty of [nanopore sequencing] is that you can see every CpG site across the HPV genome on individual viral genomes’. In one of the cell lines, FOXE1 – a potential driver for cancer transformation – was upregulated near the site of integration. Michael observed marked demethylation in and around FOXE1. Going one step further, Michael used Pore-C, an Oxford Nanopore workflow combining chromatin conformation capture with long nanopore reads. His results revealed that most of the interactions between HPV and human DNA occurred in enhancer regions. This phenomenon is consistent with the notion that HPV brings in an enhancer and interacts with other nearby genes. To further understanding of cancer phenotypes, Michael explored the full-length mitochondrial genome to begin to unpick mechanisms driving cancer energetics.
Michael’s current focus is on the most commonly aberrant human gene in cervical cancer, PIK3 – an important kinase. The drug Piqray acts as a PIK3CA inhibitor and is currently an FDA-approved drug to treat breast cancer, but its therapeutic potential for treating cervical cancer is unknown. To study this, Michael took a clinical research sample of cervical cancer cells with activation in this pathway, and treated with micromolar concentrations of the drug, which reduced expression of the immune checkpoint protein, PD-L1, reduced expression of HPV transcripts, and stopped proliferation. This would render the cancer more treatable to immunotherapies.
Both Vanessa and Michael have used nanopore sequencing to further our understanding of how HPV is driving cervical cancer transformation. From delineating complex integration events, through to methylation analysis, and chromatin conformation studies, nanopore sequencing is creating new paths to explore cervical cancer in unprecedented detail.
*London Calling 2022 hybrid conference, hosted by Oxford Nanopore Technologies; May 18–20, 2022
Oxford Nanopore Technologies, the Wheel icon, MinION, and PromethION are registered trademarks of Oxford Nanopore Technologies plc in various countries. All other brands and names contained are the property of their respective owners. © 2022 Oxford Nanopore Technologies plc. All rights reserved. Oxford Nanopore Technologies products are not intended for use for health assessment or to diagnose, treat, mitigate, cure, or prevent any disease or condition.