![Newly regenerated muscle fibers. [Joseph T. Rodgers]](https://genengnews.com/wp-content/uploads/2018/08/Apr19_2017_JosephTRodgers_NewlyRegeneratedMuscleFibers9221641057-1.jpg)
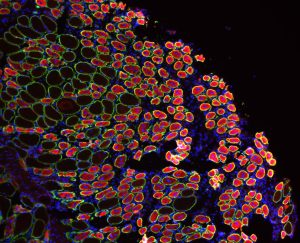
Newly regenerated muscle fibers. [Joseph T. Rodgers]
Scientists report in a paper (“HGFA Is an Injury-Regulated Systemic Factor that Induces the Transition of Stem Cells into GAlert “) in Cell Reports about a new approach to speed recovery from a wide variety of injuries.
“Our research shows that by priming the body before an injury, you can speed the process of tissue repair and recovery, similar to how a vaccine prepares the body to a fight infection,” said lead author Joseph T. Rodgers, Ph.D., who began the research during his postdoctoral studies at the Stanford University School of Medicine. He has continued his work in his current position as an assistant professor of stem cell biology and regenerative medicine at The University of Southern California.
This recent study builds upon Dr. Rodgers’ previous finding: When one part of the body suffers an injury, adult stem cells in uninjured areas throughout the body enter a primed or “Alert” state. Alert stem cells have an enhanced potential to repair tissue damage. In this new study, he identified a signal that alerts stem cells and showed how it could serve as a therapy to improve healing.
Searching for a signal that could alert stem cells, Dr. Rodgers and colleagues focused their attention on the blood. They injected blood from an injured mouse into an uninjured mouse. In the uninjured mouse, this caused stem cells to adopt an Alert state. The team identified the critical signal in blood that alerted stem cells—an enzyme called hepatocyte growth factor activator (HGFA). In normal conditions, HGFA is abundant in the blood, but inactive. Injury activates HGFA, so HGFA signaling can alert stem cells to be ready to heal.
Leveraging this discovery, Dr. Rodgers' group asked the question: What happens if HGFA alerts stem cells before an injury occurs? Does this improve the repair response? They injected active HGFA into mice that received either a muscle or skin injury a couple of days later. The mice healed faster, began running on their wheels sooner, and even regrew their fur better than mice that did not receive the HGFA booster.
These findings indicate that HGFA can alert many different types of stem cells, rousing them from their normal resting or “quiescent” state and preparing them to respond quickly and efficiently to injury, according to Dr. Rodgers.
“We believe this could be a therapeutic approach to improve recovery in situations where injuries can be anticipated,” he said, “such as surgery, combat, or sports.”
This therapeutic approach could prove particularly useful for people with impaired healing, such as older adults or diabetics.
“This work shows that there are factors in the blood that control our ability heal,” continued Dr. Rodgers. “We are looking at how HGFA might explain declines in healing, and how we can use HGFA to restore normal healing.”