March 15, 2009 (Vol. 29, No. 6)
Small Molecule Combination Therapies Are Being Investigated to Increase Response Rates
Researchers agree that now is a crucial time to be involved in hepatitis C virus (HCV) research. “Current estimates suggest that HCV infects over 170 million people worldwide,” notes David B. Smith, Ph.D., principal research scientist, Roche. “The current standard of care (SOC) for HCV involves 48–72 weeks of treatment with pegylated interferon and ribavirin. Approximately 40–60% of the patients treated with SOC achieve a sustained viral response after this treatment. Roche is highly active in the effort to discover additional treatment options that can be added to the existing SOC to increase these response rates and benefit more patients.”
Improving the course of treatment for HCV is not without its challenges, however. “HCV has a notoriously high rate of mutation,” says Anna M. Boguszewska-Chachulska, Ph.D., cofounder of Genomed. “We need to find a solution that addresses this, and there are a few compounds under development out there that look promising at this time.”
Cambridge Healthtech is hosting an HCV drug discovery track as a part of the “Drug Discovery Chemistry Conference” to be held next month in San Diego. This article previews some of the talks as well as provides an update on what’s happening in small molecule drug discovery in the HCV field.
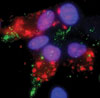
Fluorescent microscopic image of cells harboring HCV replicons
Entry Inhibitors
Flossie Wong-Staal, Ph.D., CSO and executive vp research at ItherX, says that the conference is happening at a good time for her company. “We just licensed a compound that failed as an anti-inflammatory that has great potential in the HCV space. It already has a good safety profile in over 250 human subjects and is highly potent against HCV entry (EC50 in the picomolar range). This drug is now ready for a proof of concept clinical study in HCV patients.
“Our back-up candidates exhibit EC50 of 10,000-fold therapeutic window in our assays has been shown using both genotype 1 and genotype 2 HCV. All the entry inhibitors act additively with the current standard of care as well as an HCV protease inhibitor,” says Dr. Staal. “Furthermore, the compounds are equally potent against a protease mutant virus that is resistant to the protease inhibitor. This class of compounds can add significantly to a drug cocktail targeting multiple steps of the viral life cycle, with the goal of completely eliminating virus infection.”
Dr. Wong-Staal will talk about developing entry inhibitors for HCV. “We’ve developed different programs for targeting virus entry at different points. ITX5081 and its back-up compounds target a known HCV receptor, SR-B1. We have a series of compounds that target the HCV virus envelope. This is at the lead-optimization stage. A third program is based on a new receptor for HCV that we have discovered and shown to be essential for HCV infection of liver cells.
“This target is amenable to both biologics and small molecule drug development. Unlike HIV, which utilizes one of two alternative co-receptors for virus entry, HCV engages multiple receptors in series, and it appears that blocking any of these receptors would affect virus inhibition. Furthermore, such inhibitors should be able to work synergistically with each other, as well as with inhibitors using other modes of action.”
From Bench to Bedside
NS4B plays an important role in establishing the HCV replication complex. Several key domains have been genetically validated as essential for NS4B’s function in HCV replication. This in turn has led to the development of small molecule approaches to targeting NS4B, including a new role for an old antihistamine.
Jeffrey S. Glenn, M.D., Ph.D., associate professor of medicine, department of gastroenterology and hepatology at Stanford University School of Medicine, notes that HCV poses a big clinical problem. “It’s no secret that clinical therapies right now don’t work very well,” he says. “There is a lot of room for improvement.”
And it’s quite a challenge—one of the first protease inhibitors to hit the clinic failed because of concerns about cardiotoxicity. Some compounds work well in vitro, but when tested in vivo, almost all have breakthrough resistance within a few weeks of use as monotherapy. They do have the potential to work well as a part of combination therapy, however.
Dr. Glenn works with a number of viral-specific agents. “We’re trying to increase the number of targets that can form the basis for future drug cocktails designed to maximize efficacy and decrease the emergence of resistance. We work with and have discovered a number of such novel targets, and we’re focusing on a few outside the normal range, having successfully genetically validated them.”
For example, NS4B is a protein that Dr. Glenn’s group has studied pretty extensively. “We don’t know for sure all it’s functions,” Dr. Glenn explains, “but we do know that it plays a central role in membrane-associated RNA replication—both in establishing the HCV membranous replication platform and in bringing the replicase complex components to the sites of replication. We also discovered that NS4B can specifically bind a key segment of the viral RNA and that this RNA binding is essential for HCV genome replication.”
NS4B has multiple transmembrane domain segments, threading itself in and out of the ER membrane four times, presenting a challenge to successful large-scale purification for mechanistic studies dependent on maintaining a proper topology. In vitro translation reactions with microsomal membranes can yield properly folded NS4B, but the yields are typically small.
Fortunately, however, the amounts made are sufficient for analysis using microfluidics. Dr. Glenn has initiated a collaboration with an expert in microfluidics technology to study NS4B RNA binding on the nanoliter scale. As described in their recent Nature Biotechnology paper, by screening a library enriched in previously used drugs, the colleagues identified clemizole, an antihistamine used in the 1960s, as being quite potent at specifically inhibiting NS4B RNA binding and efficacious at inhibiting HCV replication.
“Because of the extensive use in humans, we know that clemizole was extremely well tolerated in patients,” says Dr. Glenn. “We have also found in the literature a lot of the data needed for an IND package, although of course these studies were done in the 1950s and 1960s and grandfathered in, leaving some holes for what typically is found today in a modern IND filing.”
Dr. Glenn notes that for an antiviral, most researchers like to see at least 2 logs of inhibition—clemizole has only one. “But as we studied it, we noted its ability to dramatically synergize with other molecules in advanced clinical development, which makes it ideal as a future cocktail component.”
And with so few compounds able to make the final cut to drug status, there is real potential value in repurposing drugs. “There’s already been a lot published with regard to safety, we don’t have human PK data yet,” Dr. Glenn adds. “The problem is that we can’t just pull it off the shelves—it has to be made again—and as soon as we have it available, we forsee clinical trials within the year.”

Model of a peptide inhibitor binding to the NS3 helicase
NS3 Helicase Inhibitors
Dr. Boguszewska-Chachulska notes that the nonstructural protein 3 (NS3) is a highly promising target for anti-HCV therapy because of its multiple enzymatic activities, such as RNA-stimulated nucleoside triphosphatase, RNA helicase, and serine protease. The RNA helicase, the C-terminal part of NS3, is necessary for the replication of the viral RNA.
“I am mostly focused on HCV helicase inhibitors. Our group is looking for the most active and least cytotoxic, and then analyzing thoroughly their activities, such as interactions with the helicase protein,” comments Dr. Boguszewska-Chachulska, who will discuss helicase inhibitors as potential components of a multidrug therapy against HCV at the meeting.
Helicase inhibitors were identified by an in vitro fluorometric assay of helicase activity developed by Dr. Boguszewska-Chachulska’s team. “We subsequently demonstrated high antiviral activities in the HCV subgenomic replicon system, together with low cytotoxicity, for compounds belonging to three different groups: acridone-4-carboxylic derivatives (EC50 in the range of 9–10 uM), amidinoanthracyclines (EC50 in the range of 0.01–0.14 uM), and tropolone derivatives (EC50 corresponding to 30–46 uM),” she explains.
Polymerase Inhibitors
“The HCV genome encodes a number of nonstructural proteins including the NS3 protease and the RNA-dependent RNA polymerase NS5B,” notes Dr. Smith. “The polymerase is responsible for replication of the viral genome. In the cell-based replicon assay, a model for HCV infection developed by Ralf Bartenschlager, inhibitors of both the NS3 protease and the NS5B polymerase are able to suppress viral replication. Furthermore, such inhibitors have been demonstrated clinically to reduce viral load in HCV-infected patients. These two enzymes represent important targets in the development of new therapies for the treatment of HCV.”
Dr. Smith explains that 4´-azidocytidine (R1479) was discovered by Roche as a potent and selective inhibitor of HCV polymerase and advanced into early clinical development. R1479 appeared safe and showed modest efficacy in HCV infected persons. “However, exposure in humans was low and a prodrug of R1479 was developed. R1626, the triisobutyrate ester of R1479, entered Phase I studies in late 2004.”
According to Dr. Smith, R1626 showed efficacy in HCV-infected patients in Phase Ib studies, and moved into Phase II combination studies with pegylated interferon and ribavirin. While the compound proved quite efficacious, with excellent reductions in viral load and increased response rates relative to SOC, there were safety issues and development was discontinued in 2008, he said.
Nucleoside Inhibitors
“We’ve been working on nucleoside inhibitors of NS5B,” said Michael J. Sofia, Ph.D., vp, chemistry at Pharmasset. Compound R7128 is in clinical development as part of their collaboration with Roche. R7128 has gone through several clinical studies with genotypes 1, 2, and 3; patients with all genotypes have responded well to therapy. “We were the first company to demonstrate clinical efficacy in genotype 2 and 3 patients with a direct acting antiviral agent. At a 1,000 mg BID dose in combination with interferon and ribavirin we saw a rapid virological response where 90 percent of the patients went to undetectable.”
In addition, Dr. Sofia will discuss PSI-7851, a nucleoside prodrug that specifically targets treatment to the liver. “We anticipate filing an IND imminently, certainly within 1Q of 2009.”
“One of the key takeaways is that nucleosides are effective and safe agents for the treatment of HCV,” Dr. Sofia says. “They are unique among all current experimental treatments in that they show a high barrier to resistance and broad genotype coverage. We believe that they will become an integral part of any treatment regimen and certainly will be a mainstay of future therapies in the field. This is one of several strategies we have in place, as we have multiple programs in nucleosides. Our strategy is to develop proprietary combinations for treatment of HCV.”



