Researchers at Boston Children’s Hospital and collaborators have discovered that the origins of our blood may not be quite what we thought. Using cellular “barcoding” in mice, the team found that blood cells originate not from one type of precursor cell, but from two, with potential implications for the treatment of blood cancers, bone marrow transplantation, and immunology.
“Historically, people have believed that most of our blood comes from a very small number of cells that eventually become blood stem cells, also known as hematopoietic stem cells,” said Fernando Camargo, PhD, principal investigator at Boston Children’s Hospital Stem Cell Program. “We were surprised to find another group of progenitor cells that do not come from stem cells. They make most of the blood in fetal life until young adulthood, and then gradually start decreasing.”
The researchers are now following up to see if the findings also apply to humans. If so, these cells, known as embryonic multipotent progenitor cells (eMPPs), could potentially inform new treatments for boosting aging people’s immune systems. They could also shed new light on blood cancers, especially those in children, and help make bone marrow transplants more effective. Camargo and colleagues reported on their findings in Nature, in a paper titled, “Lifelong multilineage contribution by embryonic-born blood progenitors.”
Hematopoietic stem cells (HSCs) arise in the embryo from the arterial endothelium through a process known as the endothelial-to-hematopoietic transition (EHT), the authors explained. “The process generates hundreds of blood progenitors, of which a fraction go on to become definitive HSCs.” It has generally been thought that most adult blood is derived from these HSCs, and it’s not known to what extent other progenitors might also contribute to adult hematopoiesis.
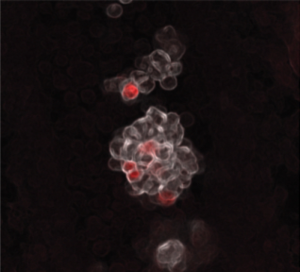
To investigate further, Camargo’s team applied a barcoding technique they developed several years ago. Using either an enzyme known as transposase or CRISPR gene editing, they inserted unique genetic sequences into embryonic mouse cells in such a way that all the cells descended from these cells also carried the inserted sequences. The team was then able to track the emergence of all the different types of blood cells—including where they came from—all the way to adulthood.
“Previously, people didn’t have these tools,” said Camargo, who is also a member of the Harvard Stem Cell Institute and a professor at Harvard University. “Also, the idea that stem cells give rise to all the blood cells was so embedded in the field that no one attempted to question it. By tracking what happened in mice over time, we were able to see new biology.”
Using their barcoding approach the researchers found that eMPPs, as compared with blood stem cells, are a more abundant source of most lymphoid cells important to the immune responses, such as B cells and T cells. “… we use in situ barcoding and classical fate mapping to assess the developmental and clonal origins of adult blood in mice,” the team explained. “Our analysis uncovers an early wave of progenitor specification—independent of traditional HSCs—that begins soon after EHT. These eMPPs predominantly drive hematopoiesis in the young adult, have a decreasing yet lifelong contribution over time, and are the predominant source of lymphoid output.”
In contrast, the team noted, “The adult HSC contribution is more prominent with age, and limited in lymphoid production.” Camargo believes the decrease in eMPPs that they observed with age may explain why our immunity weakens as we get older. “We posit here that the dynamics of the eMPP- versus the HSC-derived contribution might provide an explanation for the recognized loss of lymphoid production in aged individuals and might also underlie age-specific susceptibilities to leukemic transformation,” the team further noted.
“We’re now trying to understand why these cells peter out in middle age, which could potentially allow us to manipulate them with the goal of rejuvenating the immune system,” stated Camargo. There could, theoretically, be two approaches, either extending the life of eMPP cells, perhaps through the use of growth factors or immune signaling molecules, or using gene therapy or other approaches to make blood stem cells more like eMPPs.
Camargo is also excited about the potential implications for better understanding and treating blood cancers. For example, myeloid leukemias, which mostly impact older people, affect myeloid blood cells such as granulocytes and monocytes. Camargo thinks these leukemias may originate from blood stem cells, and that leukemias in children, which are mostly lymphoid leukemias, may originate from eMPPs. “We are following up to try to understand the consequences of mutations that lead to leukemia by looking at their effects in both blood stem cells and eMPPs in mice,” he noted. “We want to see if the leukemias that arise from these different cells of origin are different—lymphoid-like or myeloid-like.”
The recognition that there are two types of progenitor cells in the blood could, in addition, revolutionize bone marrow transplants, the researchers suggest. “When we tried to do bone marrow transplants in mice, we found that the eMPPs didn’t engraft well; they only lasted a few weeks,” Camargo pointed out. “If we could add a few genes to get eMPPs to engraft long term, they could potentially be a better source for a bone marrow transplant. They are more common in younger marrow donors than blood stem cells, and they are primed to produce lymphoid cells, which could lead to better reconstitution of the immune system and fewer infection complications after the graft.”