Scientists from Penn Medicine say they have developed the first mouse model with an idiopathic pulmonary fibrosis (IPF)-associated mutation, which induces scarring and other damage similar to what is observed in humans suffering from the condition. Their study (“Lung injury and fibrosis induced by a mutant form of surfactant protein C”) appears in the Journal of Clinical Investigation.
“No one has been able to make a model to date that actually mirrors what's going on in humans,” says senior author Michael F. Beers, M.D., a professor of pulmonary, allergy, and critical care in the Perelman School of Medicine at the University of Pennsylvania, and research director of the Penn Interstitial Lung Disease Center. “Now, we have a model that resembles the pathology, physiology, and molecular signs found in patients, which will allow us to work out new pathways and targets, and test drugs in more clinically relevant ways.”
IPF, often caught in the mid to later stages, is diagnosed in about 50,000 people a year in the U.S., and kills nearly 40,000 people during that same time. While there is no cure, two FDA-approved drugs are used to slow the disease's progression, and some patients receive lung transplants. The median survival rate is two to three years from the time of diagnosis.
Current IPF mouse models rely on a chemotherapy drug to induce an “inflammatory storm” in the lungs that creates lesions about 21 days later, Dr. Beers says. But that doesn't reflect the process that actually occurs when humans develop the disease.
In the new mouse model, the team altered a gene for making surfactant protein-C (SFTPC), which is essential for lung function. Mutations in the SFTPC gene, which are found in certain human lung cells called alveolar epithelial cells (AECs), are a promising lead for homing in on one cause of the disease, he noted.
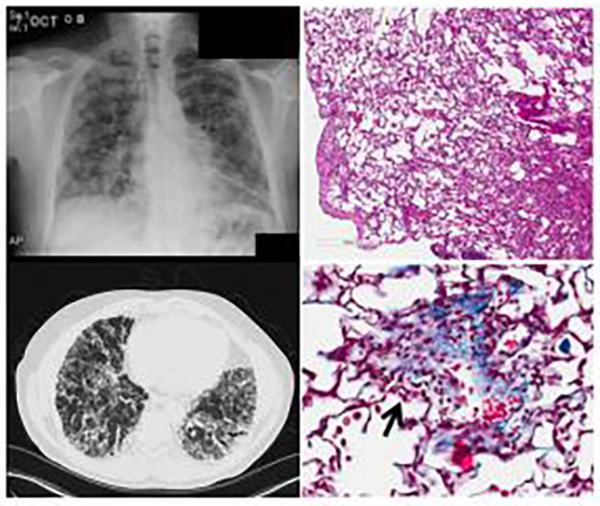
Knowing the importance of these lung AECs in the development of the disease, the team induced the SFTPC mutation into the AECs of normal mice to elicit a response. Within three days of inducing mutant SFTPC expression in adult mice, lung tissue was infiltrated by inflammatory cells; this was followed by an abnormal accumulation of inflammatory cells within tiny air sacs in the lungs.
Rapid death was also observed in 30 to 50% of the animals. Similar to what has been observed in patients, the surviving mice went on to develop progressive fibrosis and loss of lung function.
Using the new animal model, the researchers will next look at pathways that lead to the initiation and persistence of lung fibrosis.
“Now the questions become, why are those epithelial cells attracting both inflammatory cells and fibrotic cells? And how do these different cells talk to each other,” continues Dr. Beers.
“We're also taking a big data approach by profiling the genetic, proteomic, and inflammatory changes in the mice over different time points. You can't do that in humans because we see these patients once their disease has already progressed. We know very little about what happens in the beginning. This model will help answer some of those questions and hopefully lead to more effective therapeutic drugs to slow the disease.”