Lipid nanoparticle (LNP) vehicles have been crucial to the success of the Pfizer-BioNTech and Moderna COVID-19 vaccines. Without these LNP vehicles, the vaccines’ mRNA payloads wouldn’t have survived degradation within the body, and they would have had difficulty crossing cell membranes.
Having achieved such striking success with the COVID-19 vaccines, LNPs are ready for new challenges, such as improved storage, manufacturing, and delivery of mRNA vaccines of all kinds. These challenges, it should be emphasized, are global in nature. If LNPs are to succeed, vaccine stability and efficiency will have to be improved. And so, investors and innovators are making it a priority to refine both mRNA payloads and the LNP vehicles.
Ensuring stability and improving targeting
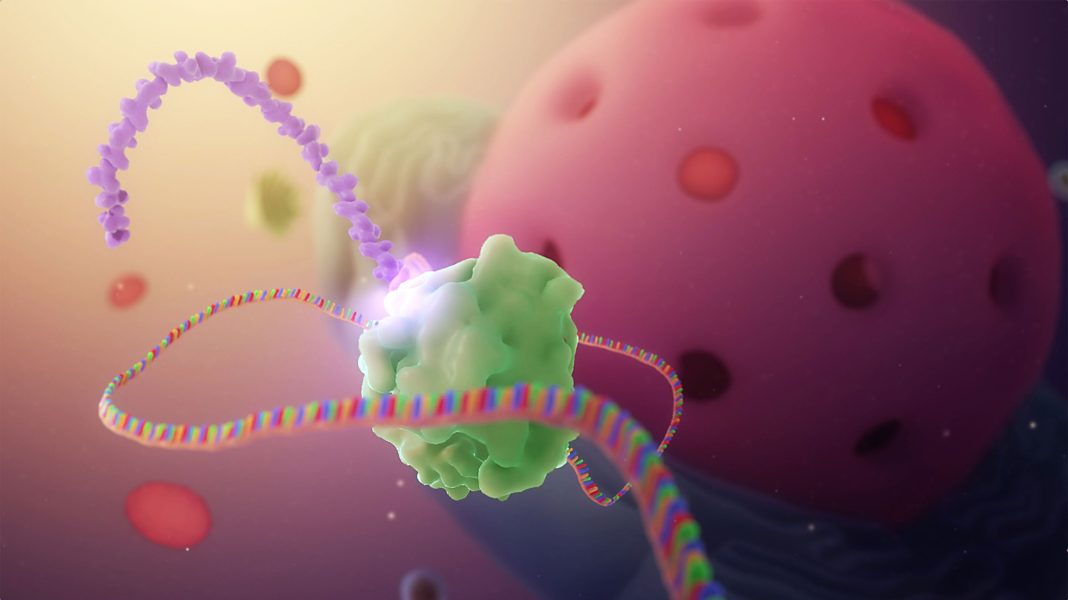
“Four different classes of lipids assemble to create a nano-fatty delivery vehicle to delivery mRNA into cells,” says Dipendra Gyawali, PhD, team lead and senior scientist for LNP process development at Moderna. “Some LNP components (ionizable lipids) facilitate mRNA encapsulation and endosomal escape.” Other components such as cholesterol and phospholipids play structural roles and help LNPs fuse with cell membranes. Finally, the addition of PEGylated lipids aids in circulation of LNPs through the body.
Moderna received emergency use authorization for its COVID-19 mRNA vaccine in December 2020. This year, the FDA gave standard approval to the vaccine, commercially known as Spikevax, for adults 18 and over. “One of the key lipids used in Spikevax is the ionizable lipid,” Gyawali notes. Ionizable lipids influence mRNA stability through counter ion production that stimulates stable complex formation between the LNP and the mRNA.
“Degradation of these bonds during storage will compromise the structural integrity of the LNP and result in poor delivery of mRNA to appropriate cell types,” he explains. “Hence, proper storage and handling of the mRNA vaccines are equally important.”
“My focus at Moderna is to understand the overall LNP formulation process and study the parameters that influence mRNA integrity,” Gyawali relates. This work involves the elimination of the reactive pathways in mRNA-LNP delivery. In a recent Nature article, Gyawali and colleagues described the formation of lipid-mRNA adducts that lead to loss of mRNA activity. “Our team developed the state-of-the-art separation method to identify this nontranslatable mRNA in LNP,” he recalls. “It also investigated the mechanism of action of this phenomenon.”
Moderna is investing in numerous proprietary LNP delivery systems for use in the clinic. According to Gyawali, the systems are being developed to “target different cell types and optimize different routes of administration.”
For respiratory illnesses such as COVID-19 and influenza, delivery of mRNA medicines directly to the lungs by inhalation is the preferred method of administration. “[This approach] maximizes the concentration of the medicine locally in the lung,” Gyawali explains. “Moderna researchers have developed a new LNP formulation aimed at addressing many of the challenges associated with lung delivery of mRNA.” Other LNP formulations studied at Moderna focus on systemic, intramuscular, and intratumoral delivery.
The LNP process development team’s research into mRNA stability has guided the development of manufacturing protocols at Moderna. “It is critical to monitor and control such degradation during the research, development, and manufacture of LNP-formulated nucleic acid products,” Gyawali points out. He adds that degradation can depend on storage conditions, trace-level impurities, cycles of process development, and intramolecular compatibility. These factors, he cautions, “can result in the loss of potency.”
A self-amplifying COVID-19 vaccine candidate
Arcturus Therapeutics believes both its STARR (self-transcribing and replicating RNA) mRNA technology platform and its LUNAR lipid-mediated delivery technology (which includes a library of 250 proprietary lipids) offer advantages in the mRNA vaccine space.
“When the COVID-19 pandemic hit, we had two mRNA-LNP products in development,” recalls Yurong Guo, PhD, director of analytical development at Arcturus. “The first, a treatment for ornithine transcarbamylase deficiency, was in Phase I trials. The second, a treatment for cystic fibrosis, was in early development. Through these programs, we accumulated significant experience in mRNA-LNP process development, analytical method development, and manufacturing, enabling the rapid transition to vaccine development.”
This April, Arcturus announced that successful results had been obtained from a Phase III efficacy trial for a COVID-19 vaccine candidate called ARCT-154. This vaccine candidate is a self-amplifying mRNA (sa-mRNA, or replicon mRNA). It includes mRNA coding for the spike protein of COVID-19 and a replicon that produces a replicase complex that prolongs the expression of the spike protein in target cells. Phase III trial data suggest that ARCT-154 is safe and stable. “With ARCT-154,” Guo remarks, “lipid nanoparticles protect mRNA from degradation and increase cellular uptake.”
All aspects of the mRNA chemistry, design, and manufacturing processes have proprietary elements. But Guo emphasizes two elements that she says are unique. The first is a proprietary cationic lipid chemistry (facilitates LUNAR LNP delivery). The second is the self-amplifying STARR mRNA (allows for much lower vaccine doses). Data from the Phase III study showed 95% efficacy at preventing severe COVID-19 disease and 55% efficacy at overall disease prevention with a 5 µg dose. “Ongoing follow-up and safety data are being collected,” Guo notes.

Arcturus has active mRNA therapeutics programs targeting ornithine transcarbamylase deficiency, cystic fibrosis, and influenza. Some of the company’s programs are being pursued with partners. For example, a program for glycogen storage disease type III involves Ultragenyx, and a program for hepatitis B involves Johnson & Johnson. Guo confirms that a self-amplified mRNA candidate will be selected for the preclinical development of the Arcturus influenza vaccine.
Evolution of the mRNA vaccine
“Up to now, the most common mRNA delivery technology has been LNP, but other approaches are emerging,” says Jeffrey Ulmer, PhD, president of TechImmune and chief scientific advisor for Immorna Biotherapeutics. He has in mind approaches such as polymers, emulsions, and higher order structures such as dendrimers.
Ulmer also sees innovations in targeting. For example, he looks forward to vaccines that are capable of targeting antigens beyond the spike protein. He says that such vaccines could “lead to cross-strain memory T cells” and reinforce efforts against COVID-19. “People working in the field basically have three options,” he points out. “We simply boost repeatedly, develop variant-based vaccines (such as influenza vaccines), or expand to using additional antigen targets.”
Ulmer suggests that with COVID-19, the inherent antigenicity of the spike protein could be why every vaccine technology that was applied to COVID-19 was effective to some degree. “[The successes against COVID-19] may create unrealistic expectations of the new technology,” he cautions. “We should be realistic about simply copying and pasting—just because it worked once for COVID-19 doesn’t mean it will work for other targets.” For successful expansion of mRNA vaccine efforts, Ulmer states, innovations in mRNA design, delivery, antigen optimization, and manufacturing quality will all be important.
As a stalwart of vaccine development, Ulmer is familiar with the history of the mRNA vaccine, which goes back to the mid-20th century. It was then that mRNA was first emulsified in LNPs. Ulmer’s first stint in the vaccine industry was between 1990 and 1998, when he served Merck as director of DNA vaccines. “Large-scale manufacturing of RNA was not considered achievable at that time, due to stability and cost,” Ulmer recalls. “But today, large-scale manufacturing at a reasonable cost is feasible.”
In 1998, Ulmer started working at Chiron Corporation, where he oversaw the development of “tools and methods focused on enabling plasmid DNA and self-amplifying mRNA technologies.” The company was bought by Novartis in 2006. Ulmer notes that Novartis “started using lipid nanoparticles to deliver mRNA because of their experience with small interfering RNA.”
Today, at TechImmune, Ulmer and his team are working on a next-generation COVID-19 vaccine that combines the benefits of antibody responses against the spike protein with CD4+ and CD8+ T-cell responses against conserved antigens to provide broad-based immunity. “We have preclinical proof of principle for the added benefit of T cells on top of antibodies,” Ulmer asserts. “We are in the midst of identifying our lead candidate consisting of spike plus one or more conserved T-cell antigens.”
Taking a global view and addressing common needs
The vaccine development market continues to see increased financial and developmental interest in the wake of the global COVID-19 pandemic. “We estimate that for the first quarter of 2022, there were 137-plus developers (across academia, industry, etc.) working on mRNA vaccines,” says Arun Kumar, PhD, vaccine development lead, Coalition for Epidemic Preparedness Innovations (CEPI). “Around 80% of these efforts were dedicated to working on SARS-CoV-2 vaccines, and 14% to working on non-SARS-CoV-2 targets.”
Multinational not-for-profit organizations, like CEPI, direct vaccine development through funding partnerships, scientific teams, and testing facilities around the globe. Efforts supported by these organizations include support for the clinical development of mRNA vaccines for influenza, Zika virus, Nipah virus, rabies virus, and HIV. “In some cases,” Kumar notes, “organizations are trying to adapt mRNA technology even where vaccines are already available to make use of RNA’s speed and scale advantages.”
Kumar indicates that the vaccine industry is focused on three specific mRNA technologies: 1) non-amplifying mRNA (unmodified and modified); 2) self-amplifying mRNA; and 3) circular mRNA.
“Most developers are working on the modified or the self-amplifying approaches,” Kumar says. Relatively few developers are using non-modified mRNA. Circular mRNA (covalently closed ring RNA) is still an emerging vaccine technology. It could increase mRNA stability, immunogenicity, and durability of protection. It could also reduce cost of goods.
“There are many gaps in mRNA vaccine technology,” Kumar notes. These gaps include stability at ultra-cold temperature, reactogenicity, and durability of protection. Another problem is that mRNA technology is limited to certain geographies. “Further work is needed to improve the technology,” he adds. “We need to make mRNA affordable and accessible for the global community.”
During the COVID-19 pandemic, the need for a vaccine was recognized almost immediately. CEPI came together with the World Health Organization (WHO), UNICEF, and Gavi to set up COVID-19 Vaccines Global Access, or COVAX, which serves as a lifeline for nations whose citizens have no other access to COVID-19 vaccines. It provides access to tools, vaccines, therapeutics, and diagnostics.
CEPI was founded in 2017. “Our original aim,” Kumar relates, “was to develop vaccines against pathogens of epidemic potential in advance of an emerging outbreak.” When COVID-19 struck, CEPI took responsibility with partners to tackle not just SARS-CoV-2, but other pathogens of pandemic potential.
“We have partnerships around the globe,” Kumar states. “We also have enabling science programs that support the vaccine development process.” With funding from governments and not-for-profit organizations such as the Gates Foundation and the Wellcome Trust, CEPI aims to scale vaccine development timelines down to 100 days. The 100 Days Mission has been endorsed by the G7 and G20 groups. CEPI supports funded partners throughout their projects, from discovery to licensure. At present, CEPI has two open calls for proposals to support mRNA innovation and thermostability of vaccines.