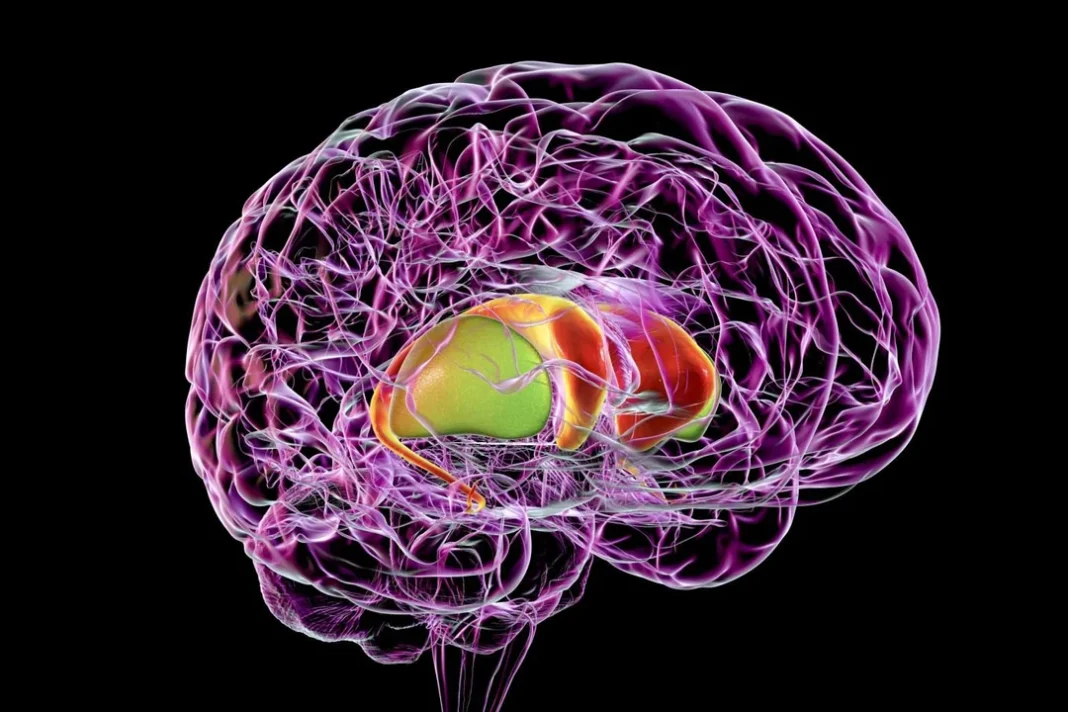
A new approach for analyzing imaging data from the striatum—a structure deep within the brain—has been developed. The approach allowed researchers to identify and quantify changes in the striatum that occur during Parkinson’s disease, paving the way for the development of a clinical tool that will allow physicians to noninvasively diagnose early-stage disease.
The researchers, led by Aviv Mezer, PhD, an associate professor at The Hebrew University of Jerusalem, used data generated by quantitative magnetic resonance imaging (qMRI). “We hypothesized that incorporating a spatial approach in qMRI methods to map the heterogeneous microstructural properties of subcortical regions, and specifically the striatum, would have important effects for our understanding of aging and Parkinson’s disease,” wrote the researchers in their article, “Mapping Microstructural Gradients of the Human Striatum in Normal Aging and Parkinson’s Disease,” which was published in Science Advances.
Parkinson’s is a progressive and debilitating disease that affects aspects of motor coordination and cognition, eventually compromising a patient’s ability to walk and even to talk. The disease can be difficult to accurately diagnose, especially in the early stages.
The new approach, developed by Mezer’s doctoral student, Elior Drori, clearly revealed biological changes in distinct regions of the striatum—the caudate nucleus and the putamen—in normal aging and in Parkinson’s disease. “In normal aging we found changes along different axes of the striatum, including asymmetry increases in anterior and posterior segments of the caudate,” the authors wrote in their article. “In contrast, the microstructural change in early-stage Parkinson’s disease was specific to posterior segments of the putamen.”
Importantly, the researchers were able to show that these changes—particularly those of the posterior putamen—were associated with motor dysfunction in the early stages of Parkinson’s disease. “We found that local alterations in the putamen constitute a signature of Parkinson’s disease,” they wrote.
The new information will not only facilitate early diagnosis of the disease, but it will provide markers for monitoring the efficacy of future drug therapies. It may also enable the identification of subgroups within the population suffering from Parkinson’s disease—some of whom may respond differently to some drugs than others—and ultimately lead to personalized treatments for patients with the disease.
“Our newly developed, automated tool for in vivo microstructural quantification is the first of its kind,” the team explained in the article. They are now developing their approach into a tool that can be used in a clinical setting. Mezer anticipates that it will be about three to five years down the line.
“What we have discovered,” said Mezer, “is the tip of the iceberg.” The team also plans to extend their new approach to investigate microstructural changes in other regions of the brain.