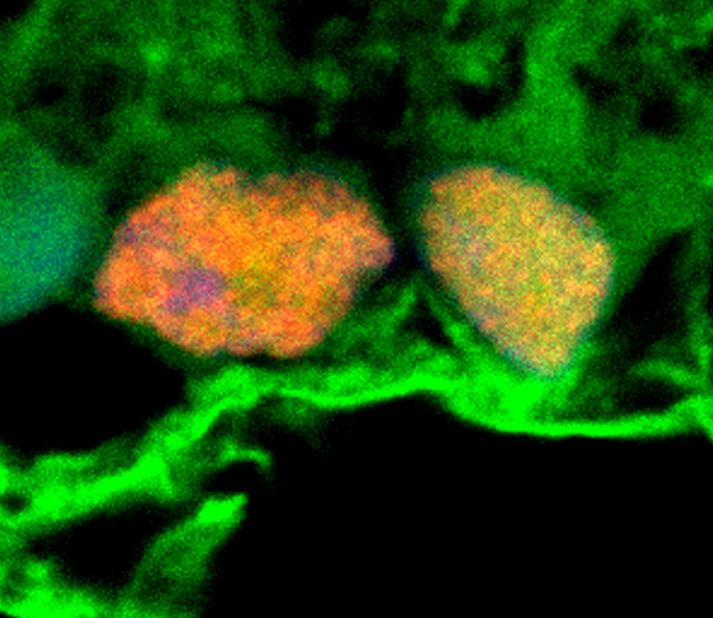
![Microscopy image shows exosomes (green) surrounding retinal ganglion cells (orange and yellow). These exosomes, which had been isolated from stem cells, were shown to convey miRNAs to the retinal ganglion cells. These miRNAs appear to have a protective effect in a model of glaucoma. [Ben Mead, Ph.D/National Eye Institute, NIH]](https://genengnews.com/wp-content/uploads/2018/08/Jan30_2017_BenMead_ExosomesSurroundingGanglionCells1341682420-1.jpg)
Microscopy image shows exosomes (green) surrounding retinal ganglion cells (orange and yellow). These exosomes, which had been isolated from stem cells, were shown to convey miRNAs to the retinal ganglion cells. These miRNAs appear to have a protective effect in a model of glaucoma. [Ben Mead, Ph.D/National Eye Institute, NIH]
Ideally, a stem cell therapy wouldn’t require the actual administration of stem cells. Even stem cells that secrete helpful compounds can lead to complications. For example, stem cells can lead to immune rejection and unwanted cell growth.
In hopes of avoiding such complications in stem cell therapies meant to protect against glaucoma and other eye diseases, scientists based at the National Eye Institute decided that they take a closer look at stem cells. The scientists, Ben Mead, Ph.D., and Stanislav Tomarev, Ph.D., knew that bone marrow–derived mesenchymal stem cells (MSCs) have been shown to protect retinal cells in models of traumatic and degenerative eye diseases. They also knew that these MSCs secrete exosomes, membrane-enclosed vesicles containing proteins, messenger RNA (mRNA), and microRNA (miRNA). Could these exosomes, Drs. Mead and Tomarev, wondered, account for the protective effects of MSCs?
The scientists decided to investigate whether exosomes released by MSCs could be taken up by retinal ganglion cells, which form the optic nerve that carries visual information from the eye to the brain. The death of retinal ganglion cells leads to vision loss in glaucoma and other optic neuropathies.
When exosomes merge with a target cells, the contents of the exosomes may spur the cell to make new proteins. Exosomes also facilitate cell-to-cell interactions and play a signaling role, prompting research into their potential therapeutic effect.
If stem cell exosomes could be administered to patients instead of whole stem cells themselves, the problems of immune rejection and unwanted cell growth could be avoided. Also, some key advantages could be gained. “Exosomes can be purified, stored, and precisely dosed in ways that stem cells cannot,” Dr. Mead said.
In a rat glaucoma model, Dr. Mead studied the effects of exosomes isolated from bone marrow stem cells on retinal ganglion cells. Exosomes were injected weekly into the rats' vitreous, the fluid within the center of the eye. Prior to injection, the exosomes were fluorescently labeled, allowing the researchers to track the delivery of the exosome cargo into the retinal ganglion cells.
The results of this work appeared January 26 in the journal Stem Cells Translational Medicine, in an article entitled, “Bone Marrow-Derived Mesenchymal Stem Cells-Derived Exosomes Promote Survival of Retinal Ganglion Cells Through miRNA-Dependent Mechanisms.” The article indicated that treatment of primary retinal cultures with bone marrow–derived MSC (BMSC) exosomes demonstrated “significant neuroprotective and neuritogenic effects.”
Exosome-treated rats lost about a third of their retinal ganglion cells following optic nerve injury, compared with a 90% loss among untreated rats. Stem cell exosome-treated retinal ganglion cells also maintained function, according to electroretinography, which measures electrical activity of retinal cells.
“Exosomes,” the article’s authors wrote, “successfully delivered their cargo into inner retinal layers and the effects were reliant on miRNA, demonstrated by the diminished therapeutic effects of exosomes derived from BMSC after knockdown of Argonaute-2, a key miRNA effector molecule.”
The researchers determined that the protective effects of exosomes are mediated by miRNA, molecules that interfere with or silence gene expression. Further research is needed to understand more about the specific contents of the exosomes, said Dr. Tomarev.
“We need to know which particular miRNA—there are more than 2000 different miRNA molecules—are delivered into the retinal ganglion cells and what proteins or signaling pathways are being targeted upon arrival,” elaborated Dr. Tomarev. “We also need to attempt to target exosomes to specific sets of neurons and other cell types or groups of cells.”
Finally, the most optimal exosome approach needs to be identified, Dr. Tomarev added. It may be that the best approach would be to combine exosomes with additional therapies. From a treatment feasibility standpoint, a lot will depend on how frequently exosomes need to be administered to achieve a therapeutic effect.