We need look no further than the addition of the Impossible Burger to Burger King’s menu to see that synthetic biology catalyzes change. But let’s look further anyway. Let’s recognize that synthetic biology can make the impossible happen in many areas besides food production. For example, synthetic biology can produce renewable fuels and manufactured goods and assist bioremediation efforts. All these applications help sustain the planet’s health. But what about our health?
It happens that synthetic biology is poised to improve our health in myriad ways, not the least of which involves the administration of novel therapeutics. Some of these therapeutics take a direct approach. They rewire the signaling pathways of human cells. But some of these therapeutics take an indirect approach. They target our microbiomes.
Here, GEN talks to three companies that have developed ingenious ways to tackle human health by targeting the bacteria in our bodies. Whether through in vivo gene editing of the existing bacteria or delivering modified bacteria with seaweed, these companies promise to make the medicines of tomorrow look very different from those of today.
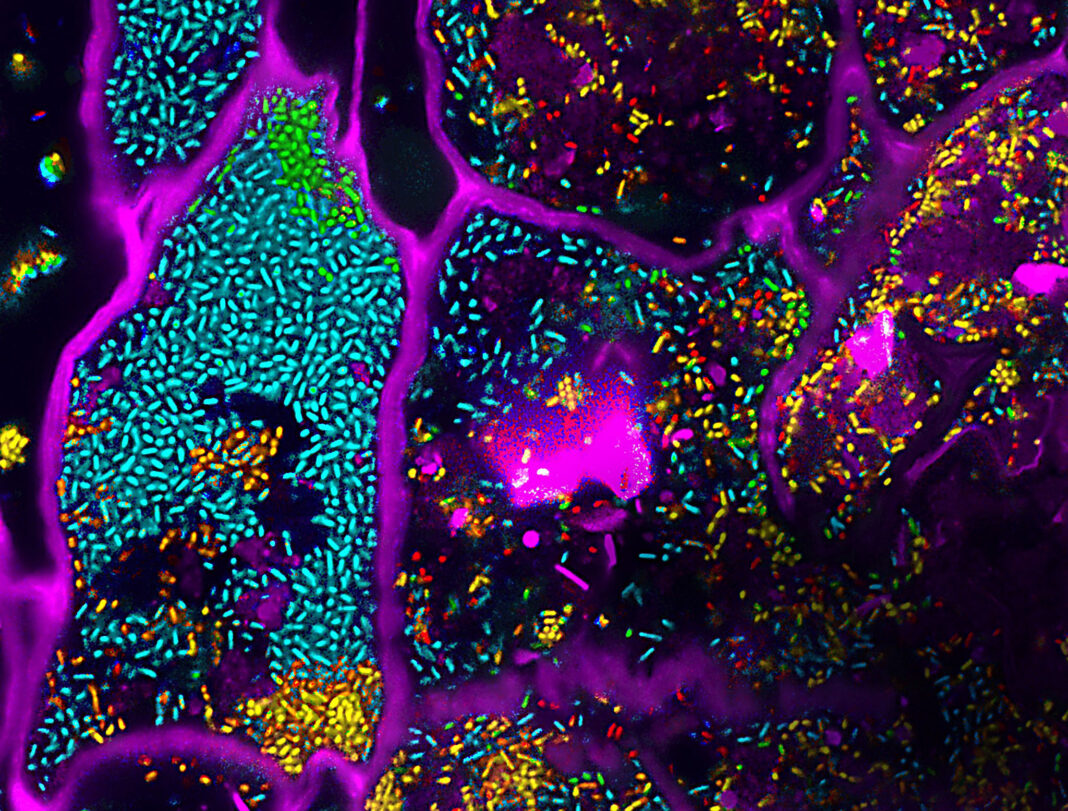
Gene therapy for the microbiome
The Paris-based company Eligo Bioscience is finding its niche while it grows and evolves. When Eligo started out in 2014, most people would have called it a phage company, or maybe a microbiome company. But now, seven years later, it is clear that Eligo hasn’t fallen into either of those buckets; rather, it is a company that combines gene editing and microbiome modification—activities that reflect the interests of the company’s two scientific co-founders. Luciano Marraffini, PhD, is a CRISPR pioneer and head of the bacteriology laboratory at Rockefeller University, and Timothy Lu, MD, PhD, is a synthetic biology powerhouse and associate professor of biological engineering and electrical engineering and computer science at MIT.
Xavier Duportet, PhD, Eligo’s CEO, likens the company to a gene therapy company targeting genes in human cells. But Eligo is targeting bacterial genes that are causative of disease. To do so, the company applies in vivo gene editing to the microbiome. The in vivo approach may bring to mind Intellia Therapeutics, but Eligo targets the microbiome, not the body’s cells.
In the past few years, there have been multiple proven examples, Duportet notes, of the expression of a specific bacterial gene and a disease. It is those genes—with a validated link between the bacterial gene and the disease—that Eligo targets for inactivation using a CRISPR-based system.
Eligo’s drugs, “Eligobiotics,” consist of a viral vector (a phage particle without the phage genome) that contains the gene editing payload, and that is specific for the bacteria being targeted. Once the CRISPR system is delivered, editing occurs in vivo, in the gut, inactivating a gene and destroying the bacteria.
One of Eligo’s candidates is being developed in a collaboration formed this past summer with GlaxoSmithKline. This candidate, EB005, is targeting a subpopulation of skin commensals, Cutibacterium acnes, that cause acne.
Another one of Eligo’s candidates, EB003, will enter a Phase I trial next year. EB003 is being developed to treat severe diarrhea induced by Shiga toxin–producing Escherichia coli (STEC). Preclinical data published earlier this year was, according to Eligo, the first time ever that a CRISPR medicine was shown to have an impact on gut disease (in relevant disease model).
Lastly, Eligo is tackling antimicrobial resistant (AMR) bacteria in a program backed by the nonprofit CARB-X. The Eligobiotic, which is designated EB004, is designed to remove AMR genes from the bacteria in the guts of patients undergoing organ transplants to prevent infection of the bacteria. A transplant patient with AMR bacteria in their gut, explains Duportet, has a 50% chance of becoming infected with the AMR bacteria after the transplant. In the case of infection, mortality jumps to 70%. If the AMR bacteria are removed, the mortality rate drops to 4%. With the Eligobiotic, the resistance genes will have been removed from the bacteria, making treatment possible.
Positive data for PKU
Interim analysis of data from two Synlogic candidates—synthetic biologics to treat phenylketonuria (PKU)—made waves at the end of September. The more advanced of the two candidates is SYNB1618, which was evaluated in the Phase II SynPheny-1 study. “[The data] represent the potentially first orally administered, safe, and efficacious therapy for PKU that would work across all types of PKU,” Aoife Brennan, PhD, Synlogic’s CEO, tells GEN. “Other oral products provide benefit only in certain genetic subtypes.”

CEO, Synlogic
The SynPheny-1 study marked the first time any gut-based approach to consuming phenylalanine (Phe) in the gastrointestinal tract of PKU patients has shown efficacy in reducing systemic plasma Phe levels. “This is the first time,” Brennan elaborates, “that a gut-based approach using engineered bacteria [produced with a synthetic biology platform] has shown a clinically relevant change in a systemic measure of disease activity.”
The data suggest that SYNB1618 lowered fasting Phe in PKU patients. The drug showed clinically meaningful reductions of Phe at several dose levels, across multiple time points, in an interim analysis of the Phase II study.
A second PKU drug, SYNB1934, showed twofold higher activity than SYNB1618 in a head-to-head Phase I study in healthy volunteers. SYN1934 is a next-generation, optimized strain with a more potent phenylalanine ammonia lyase. These unpublished data will be presented at an upcoming scientific congress. There are also plans to prepare a manuscript once final study results become available sometime next year. Based on the new data, Synlogic has incorporated SYN1934 into the trial with SYNB1618. The company will be advancing one of the two strains into Phase III based on the final results of that study.
“The first time you see data on a clinically meaningful endpoint is always the best day of the year,” Brennan declares. “It was very exciting to achieve proof of concept for the PKU program.”
The company had previously demonstrated proof of mechanism that the strains consume Phe in the gastrointestinal tract of healthy volunteers and patients, as determined by strain-specific biomarkers. But this is the first study to demonstrate proof of concept that consuming Phe in the gastrointestinal tract translates into a reduction in systemic Phe levels in plasma. This is significant because it suggests that Synlogic’s approach could have therapeutic benefit in people living with PKU.

Synlogic calls its therapeutics Synthetic Biotics. The company plans to evaluate whether they are effective against other metabolic diseases. For example, Synlogic’s SYNB8802 has shown potential as a treatment for enteric hyperoxaluria, a condition in which elevated oxalate levels may lead to kidney damage. In preclinical and Phase Ia studies, SYNB8802 showed that it had the potential to consume dietary oxalate in clinically meaningful amounts in patients with the disease.
Synthetic biology with seaweed
Synlogic is not the only company working on a treatment for enteric hyperoxaluria. This condition has also attracted the attention of Federation Bio (founded in 2019) and Novome Biotechnologies (founded in 2016). Both companies are working on programs to develop microbiome-based drugs for enteric hoperxaouria.
Federation Bio is a microbiome company that designs drugs consisting of large consortia (up to one hundred bacteria in a pill). Novome Biotechnologies takes an approach similar to that taken by Synlogic but adds a few twists. This past summer, Novome started its first Phase I trial of NOV-001, the company’s candidate for the treatment of enteric hyperoxaluria. According to Novome, this is the first therapeutic incorporating engineered colonizing gut bacteria to be evaluated in humans.
Four graduate students co-founded Novome Bio, and they still work at the company today. They include Will DeLoache, PhD, Zachary Russ, PhD, Weston Whitaker, PhD, and Liz Shepard, PhD. Today, DeLoache is Novome’s CSO, Russ is a principal scientist, and Whitaker is vice president of research, and Shepard is head of people.
In their graduate school days, DeLoache and Russ worked together in the laboratory of John Dueber, PhD, associate professor of bioengineering at the University of California, Berkeley. (The Dueber laboratory has trained many other synthetic biologists, including Tammy Hsu, PhD, the co-founder of Huue, which engineers microbes to make more sustainable indigo dyes for blue jeans.) Whitaker also worked in the Dueber laboratory before leaving to do postdoctoral work down the road at Stanford University in the laboratory of Justin Sonnenburg, PhD, associate professor of microbiology and immunology. It was there that Whitaker met Shepard.
Like other microbiome companies, Novome aims to engineer bacteria that colonize the gut to carry out functions that could help treat human disease. However, there are two characteristics that set Novome apart. The first is the company’s organism. Novome works with Bacteroides—an anaerobic, abundant, resident member of the gut microbiome. The Bacteroides delivered in Novome’s drug should be able to colonize the gut and proliferate to therapeutically relevant numbers—even if the drug is administered in small doses. But Bacteroides are not easy to genetically manipulate. (To date, genetic tools that work for Bacteroides have been harder to develop than tools that work for other bacteria.) So, Novome has its work cut out for it.
The ability of a bacterial drug to colonize the gut is a double-edged sword. Yes, it should mitigate the need for large doses. But it also introduces the challenge of maintaining control over the cell populations that have been introduced into the gut microbiome. Because Bacteroides is a resident member of the gut, safety controls need to be put into place for its growth.
Novome’s solution to this is seaweed. More specifically, Novome engineers the bacteria to metabolize porphyrin, a polysaccharide provided by seaweed, and has introduced a genetic kill switch that makes the strain’s growth dependent on the presence of the seaweed polysaccharide.
When the porphyrin is delivered as part of the drug, it is possible, DeLoache asserts, to control the number of bacteria in the patient. This system, he asserts, can eliminate transfer of the strain to untreated individuals or clearance of the strain at the end of the treatment period.
The polysaccharide must be taken every day. If doses are missed, the bacteria will disappear from the gut. The goal, notes DeLoache, is to combine the Bacteroides and the porphyrin in the same capsule, to be taken together easily, every day. The daily dose of bacteria will ensure that the patient does not become decolonized, which could happen in the event of a missed dose of porphyrin.
In its genetically engineered Bacteroides, Novome can introduce enzymatic pathways that break down toxins, produce small molecules that can be systemically absorbed, and secrete proteins that would be delivered locally in the gut. More generally, Novome’s technology delivers proteins directly to the gut—a challenging task. It is possible that this technology will be of interest to companies beyond the microbiome space. For example, some companies might repurpose Novome’s technology to facilitate drug delivery to the gut.
A gut check
Developers of synthetic biology therapeutics have scored several firsts with microbiome-modifying drug candidates: the first therapeutically engineered colonizing gut bacteria has been evaluated in humans; the first gut-based approach using an engineered bacteria has been shown to induce a clinically relevant change in a systemic measure of disease activity; the first CRISPR medicine has been shown to have an impact on gut disease. These firsts demonstrate that synthetic biology is breaking drug development barriers and preparing the way for many more therapeutic firsts in the future.