![This is a graphical schematic (left) and photograph (center) of the bilayer device showing the upper (marked with yellow lines) and lower (marked with red lines) channel separated by a semipermeable membrane. The cells are cultured on the semipermeable membrane in the upper channel of the device. Arrow shows flow direction (Scale bar: 100 µm). [Yaling Liu]](https://genengnews.com/wp-content/uploads/2018/08/112042_web1704822916-1.jpg)
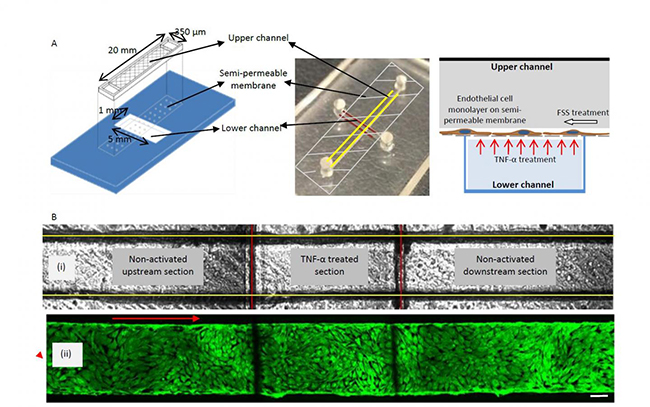
This is a graphical schematic (left) and photograph (center) of the bilayer device showing the upper (marked with yellow lines) and lower (marked with red lines) channel separated by a semipermeable membrane. The cells are cultured on the semipermeable membrane in the upper channel of the device. Arrow shows flow direction (Scale bar: 100 µm). [Yaling Liu]
The ability to recapitulate closely the cellular environment in which a new drug compound will be exposed once inside the body is the goal most scientists strive toward during the drug development process. However, creating 3D cellular systems has proven costly and cumbersome for most research laboratories.
Thus far, improvements in nanotechnology have led to better diagnostic techniques and more effective treatments for a variety of illnesses. The creation of these tiny devices enables scientists to observe cell activity and deliver drugs to individual cells—revolutionizing precision medicine for treatment of diseases such as cancer.
Nevertheless, an obstacle preventing nanomedicine from achieving its full potential is the inability to observe cell-to-cell interactions at the nanoscale in an environment that closely simulates the dynamic environment inside the body. A microfluid environment that mimics blood flow is paramount to learning how cells become damaged by disease conditions—and how they might recover in response to treatment.
Now, a team of researchers at Lehigh University and the University of Pennsylvania has developed a nanotechnique to observe cell-to-cell interaction under microfluid conditions. The investigators recently published a study describing how they successfully applied the technique to study of blood vessel inflammation, a condition closely associated with the onset of heart disease, the number one cause of death in the U.S. and globally.
“We have shown that our technique can be successfully applied to the study of inflammation and are working on a way to similarly observe and intervene in the repair of tumor cells,” explained senior study author Yaling Liu, Ph.D., associate professor of mechanical engineering and mechanics bioengineering at Lehigh University.
The findings from this study were published recently in Biofluidics in an article entitled “Biomimetic Channel Modeling Local Vascular Dynamics of Pro-Inflammatory Endothelial Changes.”
Chronic, low-grade inflammation is strongly associated with dysfunctional endothelial cells, which form the inner lining of blood vessels. The appearance of intercellular adhesion molecule-1 (ICAM-1) on the surface of endothelial cells, critical in regulating cell-to-cell interaction as part of the body's immune system response, is a sure sign that inflammation and disease are present. Therefore, observing the activation of endothelial cells under disease conditions is essential to understanding how heart disease develops and how to stop it.
The researchers looked to observe the cell-to-cell interaction beyond the limited environment associated with static cell cultures.
“We were able to mimic and observe the dynamic transfer process—that moment when the ICAM-1 antibody-coated nanoparticle binds to the cell signaling inflammation upregulation by endothelial cells—on a chip. We were also able to precisely control the flow of fluid,” noted Dr. Liu. “This reliable and relatively simple method simulates the conditions under which endothelial cells exist in the body, making it possible to observe cellular pathology in real time, and analyze differences in cells' responses to treatment.”
Because healthy cells exist on the very same chip as diseased cells, allowing for more localized control to test a particular drug, this new technology creates a platform to focus on a particular diseased region, which the investigators feel is ideally suited for testing new disease treatments. Moreover, combined with the simulated blood flow environment, this system allows researchers to gather a much more robust data set than they could by using a static culture. Using the nanoparticle probes also eliminates the need to employ radioisotope-labeled ICAM-1 antibodies to track cellular interactions– a technique that is fraught with regulatory and safety challenges.
“Our system provides a safer, less cost-prohibitive way to test a new drug in a setting that closely approximates a diseased region's environment,” Dr. Liu remarked.
The researchers are looking ahead toward plans for directly culturing patient cells in their biomimetic chip and testing under similar conditions observed in vivo, which could ultimately provide insights for precision medicine that are tailored to a specific patient under a patient specific environment.
“As we continue to develop the platform beyond the study of inflammation,” Dr. Liu stated, “we hope to make a significant contribution to the acceleration of targeted drug delivery and help usher in a new age of better medicine.”