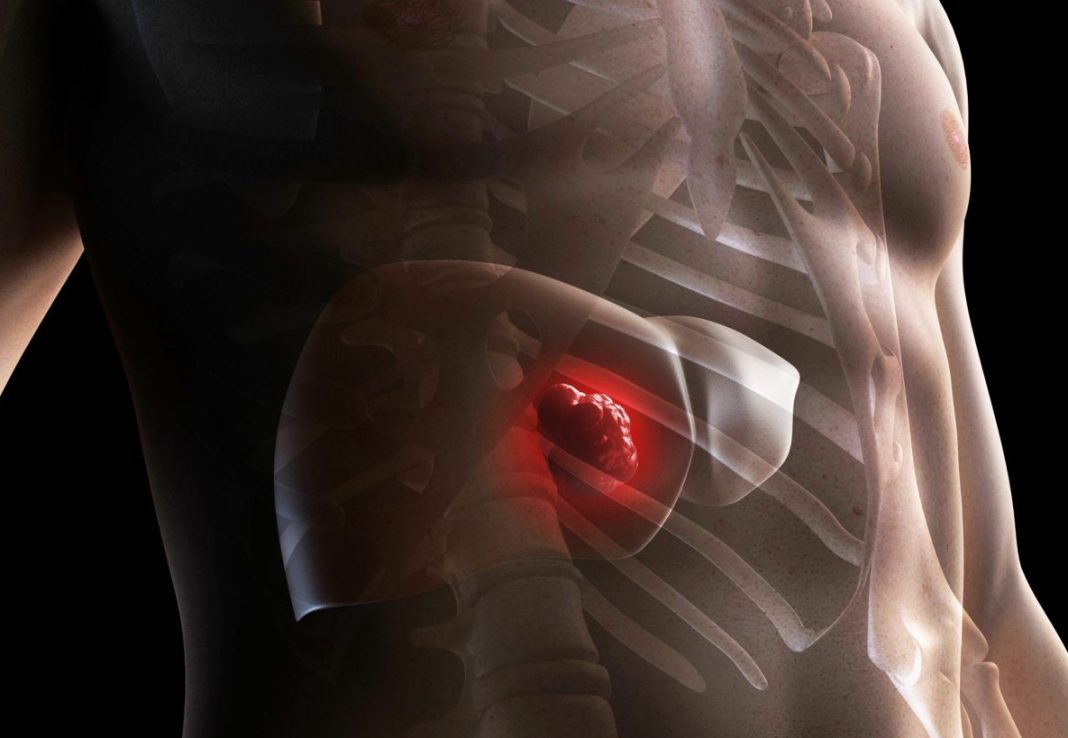
Researchers at the Perelman School of Medicine at the University of Pennsylvania have discovered that hepatocellular carcinoma (HCC) modifies its metabolism in a way that leaves it susceptible to disruptions in the supply of a key molecule, arginine. The researchers developed an approach in mice that left HCC tumors in a senescent state.
Their findings are published in the journal Cell Metabolism, in a paper titled, “GCN2 inhibition sensitizes arginine-deprived hepatocellular carcinoma cells to senolytic treatment.”
“HCC is a typically fatal malignancy exhibiting genetic heterogeneity and limited therapy responses,” wrote the researchers. “We demonstrate here that HCCs consistently repress urea cycle gene expression and thereby become auxotrophic for exogenous arginine. Surprisingly, arginine import is uniquely dependent on the cationic amino acid transporter SLC7A1, whose inhibition slows HCC cell growth in vitro and in vivo.”
“Essentially we identified a metabolic property of most liver cancers that offers the possibility of treating these cancers effectively, using drugs that are already approved or in development,” said study senior author Celeste Simon PhD, the Arthur H. Rubenstein, MBBCh professor in the department of cell and developmental biology, and scientific director of the Abramson Family Cancer Research Institute at Penn Medicine.
The approach taken by Simon and her team—targeting tumor metabolism—is one that cancer researchers have been exploring more and more in recent years.
The researchers first established from existing cancer cell gene activity databases, and from tests on patient tumor samples and cancer cell lines, that virtually all HCCs turn up their metabolism by suppressing a biochemical process called the urea cycle. The urea cycle normally produces, among other things, an amino acid called arginine, which is a building-block of proteins and has many other important functions. The researchers showed that HCC cells compensate for their loss of internal, urea-cycle arginine production by importing arginine from their surroundings, mainly via a transporter protein called SLC7A1.
Blocking SLC7A1 activity in HCC cells to starve them of arginine didn’t kill the HCC cells. Instead, arginine starvation triggered a stress response that threw the cells into a dormant, slow-growth mode—from which they could recover if arginine became available again. The researchers then tried blocking the stress response as well, and found that the HCC cells now were forced into a more profound and harder-to-reverse no-growth state called senescence.
The findings point to the possibility of a three-part combination treatment—to starve HCC tumors of arginine, to block the ensuing stress response and induce senescence, and, lastly, to kill the resulting senescent HCC cells and stop tumor growth.
“Conceivably this type of combination treatment, if implemented properly, would also make many patients more responsive to other treatments such as immunotherapies,” Simon said.