Patients with brain tumors bearing a mutant form of the enzyme IDH1 (isocitrate dehydrogenase 1) generally survive longer than patients without the mutation as such tumors are less aggressive at early stages. However, when they recur, they are more difficult to treat due to their resistance to ionizing radiation and invasive nature.
A study on human cells and a mouse model, shows a zinc finger gene (ZMYND8) that is over-expressed when IDH1 is mutated, plays a critical role in conferring radiation resistance on a subset of brain tumors. The study, conducted by researchers at the University of Michigan’s Rogel Cancer Center, was published in the journal Clinical Cancer Research on January 24th “Zinc Finger MYND-Type Containing 8 (ZMYND8) is epigenetically regulated in mutant Isocitrate Dehydrogenase 1 (IDH1) glioma to promote radioresistance.”
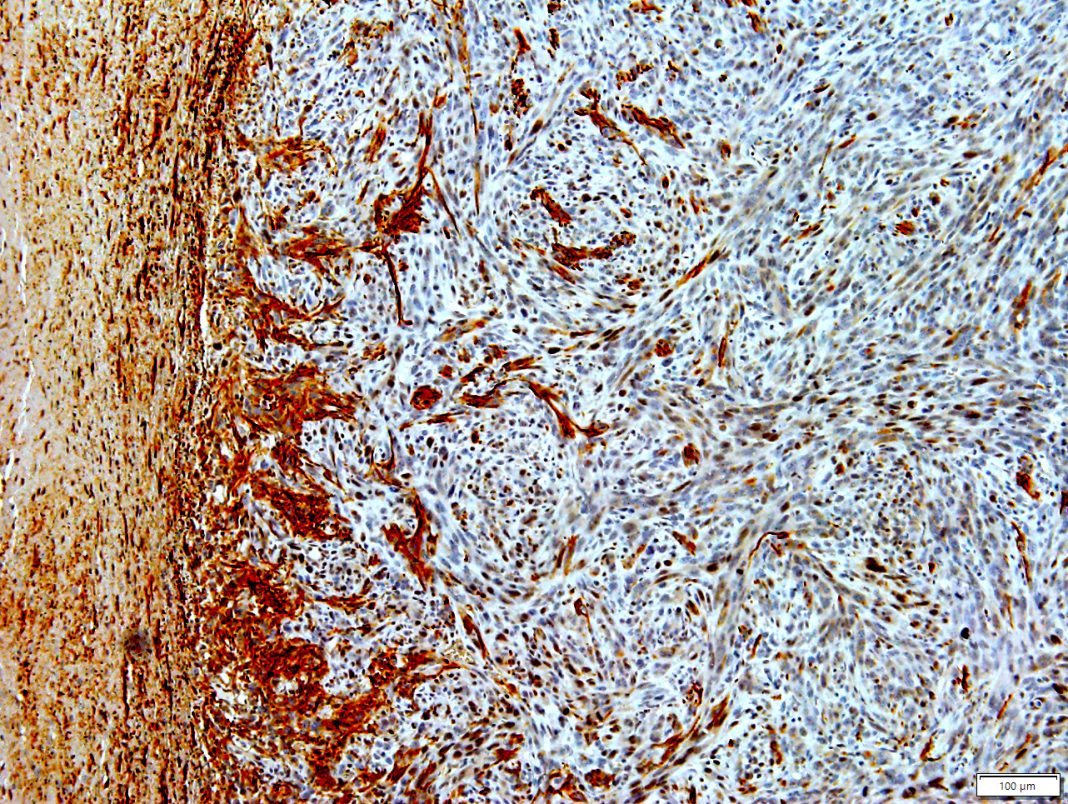
Of therapeutic significance, when researchers reduced the expression of ZMYND8 in radiation resistant glioma cells bearing mutated IDH1, the cells became susceptible to radiation-induced cell death. Mutant IDH1 changes the epigenetic regulation of chromatin, leading to hypermethylation of adult glioma. This work identifies gene targets epigenetically dysregulated by mutant IDH1 that confer resistance to radiation in glioma cells.
“These tumors almost always recur, and when they do, the tumors are much more aggressive. This finding gives us a new therapeutic avenue to treat these patients. It’s a very promising and novel therapeutic target,” said Maria Castro, PhD, professor of neurosurgery at Michigan Medicine and senior author of the study.
Glioma cell cultures bearing IDH1 mutations that the researchers used in this study were obtained from surgical biopsies of patients. The cells were treated with an inhibitor designed to block a metabolite produced by the mutated IDH1. The researchers then screened cellular mRNA and identified ZMYND8.
“After treating with the mutant IDH1 inhibitor, ZMYND8 was significantly downregulated. It’s overexpressed in mutant IDH1 glioma cells, but when you treat the cells with an inhibitor, ZMYND8 protein expression goes down. When this gene goes down, the cells become radiosensitive,” said Stephen Carney, a graduate student in the laboratory of Castro and Pedro Lowenstein, MD, PhD, also a professor of neurosurgery at Michigan Medicine.
Radiation therapy works by damaging cellular DNA and the biological role of ZMYND8 is to regulate DNA damage response. When ZMYND8 protein expression is high, researchers noted resistance to radiation. When ZMYND8 was low, radiation could successfully damage DNA in the glioma cells resulting in their death.
The results seen in human glioma cells were recapitulated in a new mouse model that the researchers developed. The mice had gliomas with mutated IDH1. The researchers found knocking out ZMYND8 in mice sensitized the tumors to radiation therapy and increased their survival.
“ZMYND8 contributes to the survival of mutant IDH1 glioma in response to radiation,” said Lowenstein. “We now have a new way of treating these tumors by using mRNA-based therapeutics in which we can downregulate the expression of ZMYND8 to render the cells radiosensitive.”
The synergistic actions of ZMYND8 knockdown in combination with other cancer drugs, such as PARP (Poly ADP-ribose polymerase) and HDAC (histone deacetylase) inhibitors further decreased resistance to radiation in the glioma cells, the researchers found. This hints at a potential for combinatorial therapy for patients with mutant IDH1 glioma.
Earlier work by the team developed synthetic protein nanoparticles (SPNPs) that can make it across the blood brain barrier. Castro intends to collaborate with colleagues at the U-M Biointerfaces Institute to design ZMYND8-inhibiting RNA, which could be delivered using these nanoparticles as vehicles.
The work was funded by the National Institutes of Health, the Pediatric Brain Tumor Foundation, Leah’s Happy Hearts Foundation, Ian’s Friends Foundation, Chad Tough Foundation, and Smiles for Sophie Forever Foundation.