A Phase II clinical trial carried out by the National Institutes of Health has found that a single dose of an antibody drug safely protected healthy, non-pregnant adults from malaria infection during an intense six-month malaria season in Mali, Africa. The antibody, designated CIS43LS, was up to 88.2% effective at preventing infection over a 24-week period, demonstrating for the first time that a monoclonal antibody can prevent malaria infection in an endemic region. Findings from the trial have just been published in The New England Journal of Medicine (NEJM) and presented at the American Society of Tropical Medicine & Hygiene 2022 Annual Meeting in Seattle.
“We need to expand the arsenal of available interventions to prevent malaria infection and accelerate efforts to eliminate the disease,” said Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases (NIAID). “These study results suggest that a monoclonal antibody could potentially complement other measures to protect travelers and vulnerable groups such as infants, children, and pregnant women from seasonal malaria and help eliminate malaria from defined geographical areas.”
NIAID sponsored and funded the trial, which was led by Peter D. Crompton, MD, MPH, and Kassoum Kayentao, MD, MPH, PhD. Crompton is chief of the Malaria Infection Biology and Immunity Section in the NIAID Laboratory of Immunogenetics, and Kayentao is a professor at the University of Sciences, Techniques and Technologies (USTTB) of Bamako, Mali. Their published report in NEJM is titled “Safety and Efficacy of a Monoclonal Antibody against Malaria in Mali.”
Malaria is a mosquito-transmitted disease caused by Plasmodium parasites. There were an estimated 241 million cases of malaria worldwide in 2020, according to World Health Organization (WHO) figures, resulting in an estimated 627,000 deaths, mostly in children in sub-Saharan Africa. These cases included more than 11 million pregnant women in Africa, resulting in an estimated 819,000 newborns with low birthweight and thus at increased risk for illness and death.
The only malaria vaccine currently recommended by WHO, called RTS,S (Mosquirix), provides partial protection against clinical malaria during the early years of life when given to children aged 5 to 17 months in four doses over a 20-month period. Other drugs consisting of small chemical compounds that effectively prevent malaria infection are also available for infants and young children as well as for travelers. “Malaria-control measures include insecticide-treated nets, early diagnosis and treatment with artemisinin-based combination therapies, and chemoprevention for high-risk groups including infants, children exposed to seasonal malaria, and pregnant women,” the researchers explained.
The requirement for frequent dosing of drugs can limit adherence, however, and the emergence of drug resistance may also limit usefulness. “Although chemoprevention is a “critically important” tool, the investigators noted, “its effectiveness may be limited by the challenge of delivering frequent treatment courses and the emergence of drug resistance.” Thus, there is an urgent need for new, fast-acting, infrequently dosed interventions that safely provide strong protection against malaria infection. “Despite these countermeasures, progress in reducing malaria cases and deaths has stalled in recent years and is further threatened by the emergence of insecticide-resistant mosquitoes and drug-resistant parasites … New tools are needed to reduce malaria morbidity and mortality and accelerate elimination efforts.”
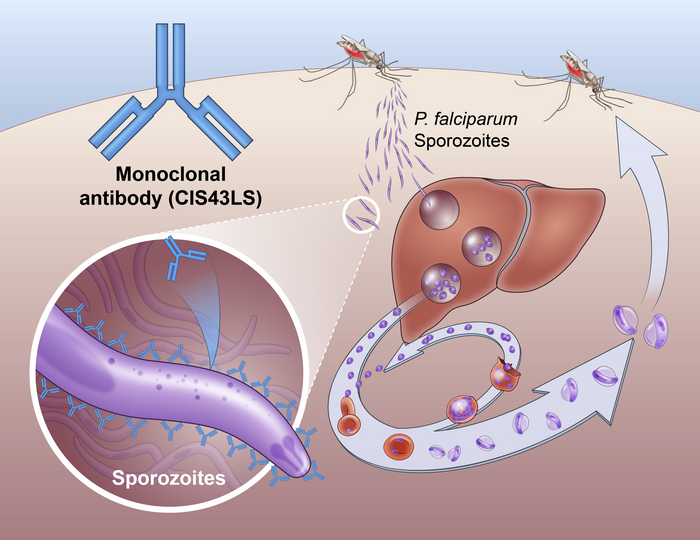
Transmission of the Plasmodium parasites that cause malaria is through the bite of an infected mosquito. The mosquito injects the parasites in a form called sporozoites into the skin and bloodstream. These travel to the liver, where they mature and multiply. Then the mature parasite spreads throughout the body via the bloodstream to cause illness. P. falciparum is the Plasmodium species most likely to result in severe malaria infections, which, if not promptly treated, may lead to death.
The reported Phase II NIAID-USTTB trial evaluated the safety and efficacy of a one-time, intravenous infusion of the CIS43LS monoclonal antibody. This antibody was previously shown to neutralize the sporozoites of P. falciparum in the skin and blood before they could infect liver cells. Researchers led by Robert A. Seder, MD, isolated a naturally occurring form of this antibody from the blood of a volunteer who had received an investigational malaria vaccine, and then modified the antibody to extend the length of time it would remain in the bloodstream. Seder is the acting chief medical officer and acting associate director of the NIAID Vaccine Research Center (VRC) and chief of the VRC’s Cellular Immunology Section.
CIS43LS targets a conserved “junctional” epitope on the P. falciparum circumsporozoite protein (PfCSP), which is the major protein expressed on the surface of the sporozoites that are transmitted by mosquitoes to humans, and is required for sporozoites to invade hepatocytes, a stage that precedes the erythrocytic stage that causes disease. So, the investigators noted, “targeting sporozoites to block infection is an approach for preventing malaria and onward transmission of the parasite.”
The reported Phase II trial enrolled 369 healthy, non-pregnant adults aged 18 to 55 years, in the rural communities of Kalifabougou and Torodo in Mali, where intense P. falciparum transmission typically occurs from July through to December each year. The trial was conducted in two parts, the investigators noted. “Part A was an open-label, dose-escalation study conducted before the malaria season to evaluate the safety and side-effect profile of CIS43LS. Part B was a double-blind, randomized, placebo-controlled trial to assess the safety and efficacy of CIS43LS,” the investigators explained.
The first part of the trial was an open-label, dose-escalation study carried out before the start of the malaria season, to evaluate the safety and side-effect profile of three doses of CIS43LS, 5 milligrams per kilogram of body weight, 10 mg/kg and 40 mg/kg. The antibody was administered by intravenous infusion in 18 study participants, with six participants per dose level.
The second, double-blind part of the trial assessed the efficacy of two different doses of CIS43LS compared with a placebo. A total of 330 participants were assigned at random to receive antibody doses of either 10 mg/kg, 40 mg/kg, or a placebo, administered by intravenous infusion. The study team followed these individuals for 24 weeks, testing their blood for P. falciparum weekly for the first 28 days and every two weeks thereafter. Any participant who developed symptomatic malaria during the trial received standard treatment from the study team.
Also, for both Parts A and B of the trial, artemether-lumefantrine was given to all the participants as a standard, directly observed treatment course at enrollment, seven to 21 days before administration of CIS43LS or placebo, to clear any possible Plasmodium falciparum bloodstage infection, the investigators further noted.
The team followed the participants in part A of the study for 24 weeks. They found that found the antibody infusions were safe and well tolerated. “In Part A, solicited local and systemic adverse events within 7 days after CIS43LS administration were all mild in severity,” they wrote. “From CIS43LS administration through the end of the 24-week study period, there were no serious adverse events, and all unsolicited adverse events were grade 1 or 2 and were considered by investigators to be unrelated to CIS43LS.”
In part B of the study, the team analyzed the efficacy of CIS43LS in two ways. In the primary efficacy analysis that was based on the time to the first P. falciparum infection over the 24-week trial period, the team found that the high dose (40 mg/kg) of CIS43LS was 88.2% effective at preventing infection, while the lower dose (10 mg/kg) was 75% effective. In the secondary efficacy analysis that was based on the Kaplan–Meier estimate of the proportion of participants infected with P. falciparum over the 24-week trial period, the team found that the high dose was 76.7% effective at preventing infection and the lower dose was 54.2% effective.
Summarizing their results in their paper, the authors reported, “In this trial, a single intravenous infusion of CIS43LS provided up to 88.2% protective efficacy against P. falciparum infection in adults over a 6-month malaria season in Mali, during which 78.2% of the participants in the placebo group became infected. These data provide proof of concept that a monoclonal antibody with an extended half-life can protect against P. falciparum infection during intense transmission for a defined time period.”
“These first field results demonstrating that a monoclonal antibody safely provides high-level protection against intense malaria transmission in healthy adults pave the way for further studies to determine if such an intervention can prevent malaria infection in infants, children, and pregnant women,” Seder said. “We hope monoclonal antibodies will transform malaria prevention in endemic regions.”
The researchers suggest that a single dose of a monoclonal antibody that prevents infection for up to six months could feasibly be administered before each malaria season for at-risk children and in early pregnancy, to complement chemoprevention and other control measures. “Overall, our trial provides field data to support the use of monoclonal antibodies as an additional intervention to complement the current arsenal of countermeasures to reduce malaria morbidity and mortality.”
Seder and colleagues have developed a second antimalarial monoclonal antibody, L9LS, that is much more potent than CIS43LS and has a longer half life. L9 can be administered in a smaller dose, and as an injection under the skin (subcutaneously), rather than by intravenous infusion. An early-phase NIAID trial of L9LS in the U.S. found that the antibody was safe and prevented malaria infection for 21 days in 15 out of 17 healthy adults exposed to P. falciparum in a carefully controlled setting. Two larger, NIAID-sponsored Phase II trials assessing the safety and efficacy of L9LS in infants, children and adults are underway in Mali and Kenya.