When COVID-19 emerged, Adarza BioSystems (like many companies) pivoted. Before the pandemic, Adarza had developed a label-free immune profiling system for cytokines and chemokines, and the company had planned for the system to serve immuno-oncology and neurology research. But after the pandemic started, Adarza adapted the system to profile SARS-CoV-2 and other viruses.
The profiling system (ZIVA™) is based on Adarza’s AIR™ (arrayed imaging reflectometry) microarray, and it measures changes in reflectivity left by biomaterials. “We made a silicon chip that is almost perfectly antireflective,” says Benjamin L. Miller, PhD, the system’s designer and chair of Adarza’s scientific advisory board. The chip is coated with probes to which label-free molecules bind.
“We don’t need a fluorescent label to detect those analytes,” Miller asserts. “Instead, we use the antireflective method.” This method measures light that leaks out. Essentially, the technology darkens the background on reflective silicon chips to enhance the “lighting up” of positive samples by a targeted laser. In published work with influenza, the technique has been used to measure up to 115 different targets on a single chip. For other applications, the technology can detect up to 200 analytes in a fluid sample.
Tech exercised pre-COVID
The technology was created by Miller, a professor at the University of Rochester Medical Center. He had worked closely with the National Institutes of Health, using AIR technology to develop new tools to monitor antibody responses to influenza and to detect and serotype the virus. Later, during a 2019 pandemic exercise, he used AIR to identify the species of human flu that was closest to the hypothetical strain used in that exercise, and thus selected the appropriate vaccine for the hypothetical pandemic.
“When COVID-19 arrived, we were well primed to think about these issues,” Miller recalls. Consequently, the company added SARS-CoV-2 proteins and subunits to its upper respiratory array, which also includes respiratory syncytial virus and varieties of influenza and other pathogens.
While the AIR technology could be used for clinical diagnosis, Adarza is positioning ZIVA, a commercial instrument based on AIR, as a research tool. “We wanted to make a high-throughput, high-definition tool for other researchers to use to understand how COVID-19 immune response interplays with individuals’ other vaccinations,” explains Bryan Witherbee, Adarza’s CEO. Later in the pandemic, he hopes ZIVA can help researchers answer questions regarding the effectivity and duration of vaccine titers, and whether those vaccines protected people from the virus.
Multiplexed antigen analysis
“What’s unique about AIR is that we’re able to look at the response to many, many antigens at once, including mutant proteins and subdomains of proteins, in one experiment,” Witherbee notes. For example, the array includes the entire Spike protein from SARS-CoV-2 and multiple subdomains such as the S1 and S2 subunits and receptor-binding domain, so researchers can understand whether antibodies are responding to any or all of those viral elements, and which antibodies are responding.
“That helps vaccine developers determine which part of the protein they could use as a vaccine element to provide the strongest response,” he maintains. Developers could also study what happens to antibody responses as the virus mutates.
“We haven’t applied for an emergency use authorization (EUA),” Witherbee notes. “The value of AIR and ZIVA is for ongoing work on therapeutic antibodies and for researchers performing analysis afterward to determine how people respond differently. We’re entering a new world where COVID-19 status is important to other diseases. There are implications for preexisting conditions and questions around whether COVID-19 brings on others.”
“Because we have the ability to ask a question in multiple different ways, any positive results are more likely to be true positives than if the question is asked only in a single way,” Miller explains.
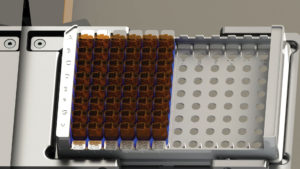
Obtaining a readout takes about 35 minutes of instrument time for an entire 96-well plate and requires only a small amount of blood, making it useful for murine tests and other situations with limited quantities of sample.
In addition to the upper respiratory infection panel, Adarza is readying an array for ZIVA that profiles cytokines. Inflammation is a huge part of all diseases, so measuring cytokines gives insights into the severity of disease and into the effect of therapeutics of interest on that disease. ZIVA’s capability in that area makes it applicable to immuno-oncology work, as well as expanding content in other research areas including neurology, metabolism, and toxicity.
Witherbee contends that AIR’s protein profiling capabilities will do for phenotypic analysis what the genome revolution did for genomic analysis. He says that in the not-so distant future, “Putting together large amounts of genotype and phenotype information from individuals will become common practice, fully enabling precision medicine.”
From Rochester to St. Louis
Adarza was formed in 2008 from the early efforts at the University of Rochester but really came into its own in 2018 as the company translated the initial invention into a complete package with the instrument, analysis function, and consumables. Along the way, adds Witherbee, “We made it user-friendly.” That meant combining analyte detection, optics, a camera, and a means of washing and drying biosensors in the Ziva system to create a fully automated workflow that performs many serology testing steps in parallel.
Now Adarza is headquartered in St. Louis—“a gem in the Midwest,” Witherbee declares—where it draws on a talent pool of scientists and engineers experienced with Pharmacia and Pfizer, as well as Monsanto, Boeing, and other tech-savvy organizations in the area. “St. Louis supports innovation and science, and people come here and love it,” he says.
As does any company with a new product, Adarza has an installed base that is still small. Also, as Witherbee admits, “We were a little late to the [COVID-19] party.” Having a larger base or developing the viral panel earlier could have helped researchers during the pandemic, he notes.
Adarza is working to remedy that this fall as it on-boards early-access customers for its viral panel and its cytokine and chemokine offerings. Witherbee plans a full commercial launch of the ZIVA system in early 2021, later than initially expected but, with COVID-19, somehow right on time.

