Circulating tumor cells (CTCs) are epithelial cells usually found in cancer patients’ blood, albeit in very small numbers. This week, scientists reported that these cells undergo a “personality” change, or shift from their original adherent state to a migratory mesenchymal state.
This “epithelial-mesenchymal transition,” or EMT, involves a variety of changes to the cell, including their expression of specific proteins, allowing it to sever its connections with nearby cells, wandering through the bloodstream and forming new tissues. Studies in cell lines and mice have suggested that this transition also plays a role in cancer metastasis.
In the February 1 issue of Science, researchers from Harvard Medical School, Charlestown, MA, and the Howard Hughes Medical Institute, Chevy Chase, MD, reported that they had analyzed isolated CTCs from breast cancer patients for their expression of epithelial and mesenchymal markers.
Cells expressing both types of markers were rare in primary breast tumors but enriched among circulating tumor cells, as were cells expressing only mesenchymal markers. Mesenchymal CTCs occurred as both single cells and multicellular clusters, expressing known EMT regulators including transforming growth factor (TGF)-β pathway components and the FOXC1 transcription factor.
Serial blood samples from one patient revealed that circulating tumor cells in the mesenchymal state declined in number when the patient responded to therapy but rebounded when the disease began to progress again—a pattern repeated when a different therapy was administered.
The authors said that EMT had been implicated in this process based on studies with human cancer cell lines and mouse models, but to date, immunohistochemical approaches to identify EMT in tumors has been complicated by the presence of reactive mesenchymal stromal cells.
The presence of reactive mesenchymal cells, they said, has hampered analysis of CTCs because of reliance on epithelial markers to separate cancer cells from surrounding hematopoietic cells of mesenchymal origin.
To overcome these technical challenges, the authors optimized microfluidic capture of CTCs with epithelial- and tumor-specific antibodies, then used this technology to analyze EMT in CTCs from breast cancer patients.
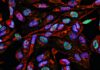
The authors developed a quantifiable, dual-colorimetric RNA-in situ hybridization (ISH) assay to examine tumor cells for expression of seven pooled epithelial transcripts, probes that were validated in cell lines to confirm differential expression in epithelial versus mesenchymal cancer cells, and the absence of expression in blood cells that contaminate CTC preparations.
After validating the E/M RNA-ISH analysis in mouse xenografts of epithelial or mesenchymal breast cancer cells, the scientists applied the assays to primary human breast cancer specimens.
The authors concluded that the clinical significance of EMT as a potential biomarker of therapeutic resistance and as a potential drug target in breast cancer should be further investigated.