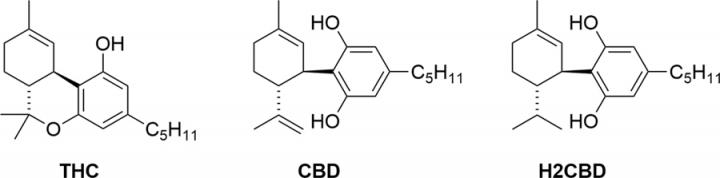
Scientists at the University of California (UC), Davis, and the University of Reading, U.K., have chemically synthesized a non-psychoactive analog of the marijuana compound cannabidiol (CBD), which was as effective as the plant-derived CBD at treating induced seizures in experimental rats. The researchers say the process for synthesizing 8,9-dihydrocannabidiol (H2CBD) is simple, scalable, and cheap, and could avoid the legal complications associated with cannabis-derived products. And unlike CBD itself, H2CBD can’t easily be converted to the psychoactive cannabinoid tetrahydrocannabinol (THC).
“It’s a much safer drug than CBD, with no abuse potential and doesn’t require the cultivation of hemp,” commented Mark Mascal, PhD, a professor in the UC Davis department of chemistry. The UC Davis and University of Reading team reported their development and in vivo tests in a paper in Scientific Reports, which is titled, “Synthetic, non-intoxicating 8,9-dihydrocannabidiol for the mitigation of seizures.”
CBD is the second most abundant cannabinoid found in the hemp plant Cannabis sativa. The compound is being studied widely for its potential therapeutic effects against a wide range of diseases and disorders, including anxiety, glaucoma, epilepsy, spasticity, inflammation, neurodegenerative diseases, affective disorders, and cancers, the researchers wrote. However, any potential medical benefits of cannabis-derived cannabinoids, and in particular CBD, must be assessed in the context of potential disadvantages, they continued, “including adverse health effects, potential for abuse, cognitive and motor impairment, psychiatric disturbances, legal issues, and the environmental impact of marijuana cultivation.”
THC, the most abundant cannabinoid in marijuana, is largely responsible for the intoxicating effects of the drug, and can also cause other adverse effects including ataxia and tachycardia. While the use of purified CBD could help to get around the potential health concerns associated with using THC-containing cannabis plant extracts, but there are still issues, the researchers pointed out. All marijuana extracts, including CBD, are controlled substances in most countries, even though some have decriminalized cannabis used for therapeutic purposes.
CBD also has to be extracted from the marijuana plant, and so may contain impurities and other contaminants, including pesticides. And even given the availability of pure CBD, it is “technically trivial” to convert CBD to THC. “Pure THC, containing no CBD to antagonize its psychotropic effects, is a potentially dangerous drug,” the authors commented. “Were CBD to become freely available, it could lead to a culture similar to that of the pseudoephedrine-to-methamphetamine ‘meth lab’ phenomenon, except that conversion of CBD to THC would involve a logistically far simpler chemical transformation.”
The potential use of cannabis as an anti-epileptic is a particularly high profile area of therapeutic research, the team pointed out. Historical and anecdotal evidence, together with a few reported case studies, have suggested the “practically unique” effectiveness of cannabis against some cases of epilepsy that haven’t responded to conventional therapies. FDA recently approved a purified herbal CBD, Epidiolex, for treating Lennox-Gastaut, and Dravet syndromes, which are both severe forms of childhood epilepsy.
The UC Davis and Reading team now reports on the synthesis of H2CBD from easily and cheaply available chemicals, using a simple, one-step process. Importantly, they point out, H2CBD isn’t found in cannabis extracts, and so is not currently a controlled substance, and the synthetic compound also can’t easily be converted to THC. The ability to synthesize H2CBD in the lab would also negate the need to grow cannabis as a crop. “Preparation of H2CBD from readily available, non-cannabis-based precursors eliminates the necessity to cultivate marijuana and its attendant social and environmental concerns,” they added.
To evaluate the anticonvulsive properties of H2CBD the researchers tested the compound in a rat model of chemically-induced epilepsy. The results showed that pretreating animals using H2CBD was just as effective as pretreatment using an equivalent dose of cannabis-derived CBD at inhibiting seizures triggered by the convulsant drug pentylenetetrazole (PTZ). “These results unequivocally demonstrate that H2CBD exhibits a dose-dependent anticonvulsant action in acute, PTX-induced generalized seizures in rats, with a maximal protective effect comparable to a matching dose of the established anticonvulsant CBD,” the authors concluded.
They acknowledge that further studies will be needed to evaluate H2CBD further. Even so, they wrote, “… assuming the principal medical justification for pursuing cannabis-based therapies is their extraordinary anticonvulsant activity, and that all other indications (anxiety, chronic pain, nausea, anorexia, etc.) can be effectively managed with non-controversial drugs, H2CBD may find application as a safer alternative in terms of its lack of abuse liability and absence of psychotropic effects.”
Mascal’s group is now working with colleagues at the UC Davis School of Medicine to carry out further studies with H2CBD, with a view to moving into clinical trials soon. UC Davis has applied for a provisional patent on the antiseizure use of H2CBD and its analogs, and Mascal has founded a company, Syncanica, to continue development of the compound.







