Psychedelic drugs such as LSD, psilocybin, and mescaline cause severe and often long-lasting hallucinations, but they also show great potential in treating a number of serious psychiatric conditions, such as major depressive disorder. The results of new research headed by scientists at the University of California at Chapel Hill School of Medicine, and Stanford University School of Medicine, have now for the first time solved the high-resolution structure of these psychedelic compounds when they are actively bound to the 5-HT2A serotonin receptor (HTR2A) on the surface of brain cells. These new insights could feasibly help scientists to discover selective, non-hallucinogenic drugs that can be used to treat a range of neuropsychiatric disorders. It may also be possible to alter the chemical composition of drugs such as LSD and psilocybin—the psychedelic compound in mushrooms that has been granted breakthrough status by FDA to treat depression.
“Millions of people have taken these drugs recreationally, and now they are emerging as therapeutic agents,” said Bryan L. Roth, MD, PhD, who is the Michael Hooker Distinguished Professor of Pharmacology at the University of North Carolina School of Medicine, and co-senior author of the team’s published paper in Cell. “Gaining this first glimpse of how they act at the molecular level is really important, a key to understanding how they work. Given the remarkable efficacy of psilocybin for depression (in Phase II trials), we are confident our findings will accelerate the discovery of fast-acting antidepressants and potentially new drugs to treat other conditions, such as severe anxiety and substance use disorder.”
Roth, together with co-senior author Georgios Skiniotis, PhD, at Stanford, and colleagues, report on their findings in a paper titled, “Structure of a Hallucinogen-Activated Gq-Coupled 5-HT2A Serotonin Receptor.”
Hallucinogens such as lysergic acid diethylamide (LSD), psilocybin, and substituted N-benzyl phenylalkylamines are used widely recreationally, and some, such as psilocybin and LSD, have been described to have potential therapeutic activity against many neuropsychiatric diseases, such as depression, anxiety, and substance abuse, the authors noted. “Psilocybin, for instance, has shown efficacy in two Phase II clinical trials of depression and anxiety,” the team reported. “Likewise, LSD has been reported inpilot studies to have efficacy in cluster headaches, to alleviate anxiety in terminal illness, and a number of uncontrolled and anecdotal reports have suggested its therapeutic actinos in other neuropsychiatric disorders.”
Despite this evidence, little is known about the underlying mechanisms in the brain by which such drugs induce their hallucinogenic, and potentially therapeutic effects. To fully investigate how these drugs work, scientists need to know how the compounds interact with brain cells at the molecular level to cause their dramatic biological effects.
Scientists believe that activation of the 5-HT2A serotonin receptor (HTR2A) is key to the effects of hallucinogenic drugs. “These receptors are expressed at very high levels in the human cerebral cortex,” said Roth, who holds a joint faculty appointment at the UNC Eshelman School of Pharmacy. “When activated, the receptors cause neurons to fire in an asynchronous and disorganized fashion, putting noise into the brain’s system. We think this is the reason these drugs cause a psychedelic experience. But it isn’t at all clear how these drugs exert their therapeutic actions.”

For their newly reported study, Roth’s lab collaborated with Skiniotis, a structural biologist at the Stanford University School of Medicine. “A combination of several different advances allowed us to do this research,” Skiniotis said. “One of these is better, more homogeneous preparations of the receptor proteins. Another is the evolution of cryo-electron microscopy technology, which allows us to view very large complexes without having to crystalize them.”
Roth credits co-first author Kuglae Kim, PhD, a postdoctoral fellow in his lab, for steadfastly exploring various experimental methods to purify and stabilize the very delicate serotonin receptors. “Kuglae was amazing,” Roth said. “I’m not exaggerating when I say what he accomplished is among the most difficult things to do. Over three years in a deliberate, iterative, creative process, he was able to modify the serotonin protein slightly so that we could get sufficient quantities of a stable protein to study.”
The research team used Kim’s work to reveal the first X-ray crystallography structure of LSD bound to HTR2A. Importantly, Stanford investigators then used cryo-EM to uncover images of a prototypical hallucinogen, called 25-CN-NBOH, bound together with the entire receptor complex, including the effector protein Gαq. In the brain, this complex controls the release of neurotransmitters and influences many biological and neurological processes.
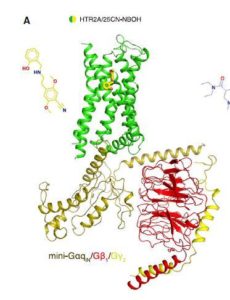
The cryo-EM image is like a map of the complex, which Kim used to illustrate the exact structure of HTR2A at the level of amino acids. “Because the 5-HT2A receptor is essential for the actions of classical psychedelics including LSD, psilocin, mescaline, and various N-BOH analogs, these studies provide structural insights into the actions of psychedelics at their molecular target,” the team wrote.
“In addition to these fundamental insights into GPCR-Gq interactions, our findings have relevance for neuropsychiatric drug discovery. Psilocybin and LSD have emerged as potential therapeutics for a number of neuropsychiatric conditions including depression, anxiety, substance abuse, and cluster headaches. Because the 5-HT2A receptor is essential for the actions of psilocybin in humans, insights into the molecular details of both HTR2A ligand recognition and HTR2A-effector coupling are key to arriving at a molecular understanding of hallucinogen actions.
Roth, a psychiatrist and biochemist, leads the Psychoactive Drug Screening Program, funded by the National Institute of Mental Health. This gives his lab access to hallucinogenic drugs for research purposes. Normally, these compounds are difficult to study in the lab because they are regulated by the Drug Enforcement Agency as Schedule 1 drugs. “One of the main goals of my work is to understand how hallucinogens exert their actions on the brain,” he noted. “If we can understand how they work at the molecular level, this will ultimately give us clues into human consciousness, perception, and awareness.”

Roth and colleagues are now applying their findings to structure-based drug discovery for new therapeutics. One of the goals is to discover potential candidates that may be able offer therapeutic benefit without the psychedelic effects.
“Given the potential therapeutic actions of hallucinogens, these findings could accelerate the discovery of more selective drugs for the treatment of a variety of neuropsychiatric disorders,” the team concluded. “… these studies will provide a framework for a structure-guided search to identify more selective and efficacious HTR2A agonists as potential innovative neuropsychiatric therapeutics as recently exemplified by us for other GPCRs,.” Skiniotis further remarked, “The more we understand about how these drugs bind to the receptors, the better we’ll understand their signaling properties. This work doesn’t give us the whole picture yet, but it’s a fairly large piece of the puzzle.”