Some kids suffer repeated bouts with step throat and tonsillitis, whereas other kids seem relatively immune. What accounts for the differences in susceptibility? Unfortunately, investigating this question is harder than asking kids to say, “Ah.” Answers are, potentially, at the immunological and genetic levels. Taking up the challenge of peering into these depths, scientists based at the La Jolla Institute for Immunology have found evidence that group A Streptococcus recurrent tonsillitis (GAS-RT) is a multifactorial disease.
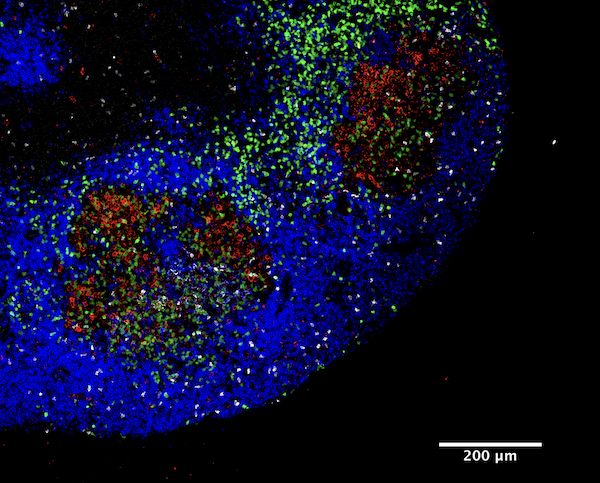
The scientists, led by clinical associate Shane Crotty, PhD, observed that the GAS-RT tonsils had smaller germinal centers—sites where B cells and T cells interact—and GAS-RT blood samples displayed lower amounts of antibodies against a GAS bacterial toxin named SpeA. These tonsils also harbored fewer germinal center T follicular helper cells, which orchestrate the immune response to GAS infection. Interestingly, the authors identified two variations in human leukocyte antigen genes that were associated with a higher risk of RT, indicating that some children may be genetically predisposed to the disease.
Although they acknowledge that further research is necessary, the La Jolla scientists are optimistic that their findings could facilitate the development of new vaccines for RT and strep throat that target SpeA—potentially reducing childhood strep throat disease burden by avoiding costly RT antibiotics treatments and surgeries.
Detailed findings appeared February 6 in the journal Science Translational Medicine, in an article titled, “Recurrent group A Streptococcus tonsillitis is an immunosusceptibility disease involving antibody deficiency and aberrant TFH cells.” The article described the phenotypic, genotypic, and functional studies that were conducted on tonsil samples taken from a total of 146 children aged five to 18 years old. All the children had undergone tonsillectomies for either GAS-associated RT or sleep apnea.
“By integrating immune profiling and clinical data with transcriptomic and functional analyses, we revealed immunologic features of GAS RT that provide evidence that RT is an immunosusceptibility disease,” the article’s authors wrote. “We observed that RT tonsils have significantly lower GC-TFH cell frequencies; RT children have impaired anti-SpeA antibody titers, which have been associated with protective immunity to GAS; specific HLA class II alleles were associated with RT; and SpeA can induce GzmB expression in GC-TFH cells.”
Although RT is surely a multifactorial disease, the La Jolla scientists noted, the current findings suggest that the sporadic nature of RT is linked to HLA-associated genetic susceptibility differences with HLA class II allelic variants affecting GAS superantigen binding.
Strep throat, which causes approximately 600 million cases a year, occurs when GAS bacteria infect the throat and cause fever, swelling of the tonsils and enlarged lymph nodes. Most cases can be treated with antibiotics, but some infected children develop RT, which results in hundreds of thousands of school absences each year and often leads to tonsillectomies, an invasive procedure in which the afflicted tonsils are removed.
“We have 100+ years of experience with this disease but there really wasn’t any good explanation why some kids suffer from recurrent strep throat,” said Crotty. “We think that this is the first solid evidence that there is an important immunological component as well as a genetic one which together contribute to recurrent strep throat. Let’s try and build on it.”
Short for streptococcal pyrogenic exotoxin, SpeA is not an essential component of the GAS genome. However, a particularly potent version of the toxin arose in the bacteria in the 1980s and these strains quickly swept the globe to become the most prevalent cause of strep throat. Children in the control group had high anti-SpeA antibody titers, which indicated that they had been exposed to the bacteria but did not get sick.
Among children with recurrent GAS tonsillitis, the disease was likely to run in the family, suggesting a genetic component. Genetic testing revealed two specific genetic variants in the HLA region, which determines how pathogens interact with the immune system, that were associated with increased susceptibility to recurrent tonsillitis and one that protected against the disease.
“Since the immunological connection, as well as the genetic connection, are all tied to an insufficient antibody response against SpeA it suggests that recognizing this factor is actually a key problem for these kids,” noted Crotty. “Having a vaccine that trains the immune system in advance might be able stimulate a protective immune response that can prevent recurring bouts of tonsillitis.”