Researchers in the U.S. have found evidence of the infectious agent that causes sporadic Creutzfeldt-Jakob Disease (sCJD) in the eyes of deceased patients. The discovery could lead to the development early diagnostic tests for the disease—which is caused by abnormal forms of normally harmless prion proteins—but also suggests that the disease might be transmitted through procedures such as corneal grafts.
“Almost half of sCJD patients develop visual disturbances, and we know that the disease can be unknowingly transmitted through corneal graft transplantation,” explained Christina J. Sigurdson, DVM, Ph.D., professor of pathology at the University of California (UC) San Diego and UC Davis. “But distribution and levels of prions in the eye were unknown. We’ve answered some of these questions. Our findings have implications for both estimating the risk of sCJD transmission and for development of diagnostic tests for prion diseases before symptoms become apparent.”
The studies, carried out by UC San Diego and UC San Francisco scientists in collaboration with a team a the National Institutes of Health (NIH), are reported in mBio, in a paper titled, “Prion seeds distribute throughout the eyes of sporadic Creutzfeldt-Jakob disease patients.”
Prion diseases occur when misshapen prion proteins accumulate in the brain and cause lesions that can lead to progressive neurodegeneration. CJD is the most common prion disease in humans, and is classified as sporadic, familial, or iatrogenic (caused by a medical treatment or procedure). While many people are aware of the very rare cases caused by eating beef that has been infected by a similar disease, bovine spongiform encephalopathy, or “mad cow disease,” about 85% of cases of CJD are sporadic, with patients having no known risk factors. About another 10–15% of CJD cases in the U.S are hereditary and linked with genetic mutations. In acquired CJD the prions are transmitted through medical procedures such as corneal grafts.
Previous studies have shown that the eyes of CJD patients can contain infectious prions, but what isn’t yet understood is the distribution of prions in the different tissues of the eye. The risk of iatrogenic prion transmission through ophthalmic procedures isn’t known, but there have been probably cases, the authors pointed out. “Corneal grafts from prion-infected patients have led to two probably and three possible cases of iatrogenic prion transmission.” The risk of transmission through ophthalmic procedures is particularly relevant given the rise in corneal transplantation surgery worldwide. In the U.S., for example, about 64,000 corneal transplants are carried out per year.
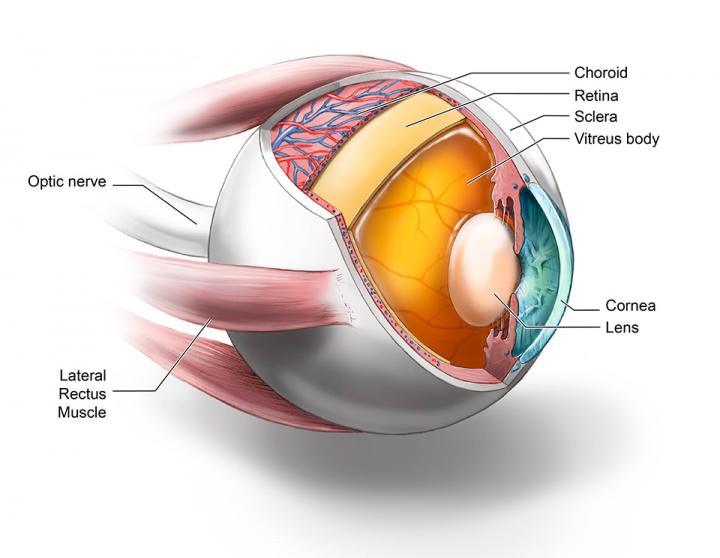
The researchers used the highly sensitive and quantitative real-time quaking-induced conversion (RT-QuIC) assay to look for prion seeding in eight different ocular tissues, including the cornea, lens, ocular fluid, retina, and optic nerve, in the post-mortem eyes of 11 patients who had died from sCJD. The RT-QuIC technique was developed by co-researcher Byron Caughey, Ph.D., at the NIH Rocky Mountain Laboratories in Montana, and is used by clinicians to diagnose sCJD in people, commonly through cerebrospinal fluid and nasal brushings.
Used to analyze the CJD patient eyes, the assay detected abnormal prions in multiple ocular tissues, with the highest seed levels—which in some cases were not much lower than those in the brain—found in the retina. “We found that all 11 sCJD patient eyes were positive for prion seeding activity and showed the highest seeding activity in the retina,” they wrote. “Prion seed levels in the retina were significantly higher than the extraocular muscles, optic nerve, cornea, lens, vitreous fluid, and sclera.”
The team says that as well as suggesting a potential diagnostic utility, their results also highlight ophthalmic surgery as a possible biohazard, and support recommendations for the use of disposable instruments or decontamination procedures to prevent iatrogenic prion transmission. “Our findings support the World Health Organization classification of eye components as having high prion infectivity and have implications for patient safety,” they noted. “As the early-disease phase of sCJD often includes visual symptoms, patients with sCJD will often have diagnostic assessments performed by an ophthalmologist, potentially contaminating instruments.”
The researchers aim to continue their work evaluating whether examining eye tissues and fluids using RT-QuIC could represent a diagnostic route for other neurodegenerative diseases characterized by the abnormal accumulation of proteins. “Because other protein aggregates such as amyloid-β, α-synuclein, and tau may also spread from brain to retina, it would also be important to continue to evaluate eyes from patients having more common neurodegenerative diseases, such as Alzheimer’s disease, synucleinopathies, and tauopathies, particularly in light of recent findings showing the prion-like spread of protein aggregates through the CNS.”