Cancer immunotherapy drugs are designed to stimulate the immune system to attack tumors. These treatments can work well against some types of cancer, but have shown mixed success against lung cancer. A new study by researchers at the Massachusetts Institute of Technology (MIT) has shed light on why the immune system mounts such a lackluster response to lung cancer, even after treatment with immunotherapy drugs. The team’s research, in mice, showed that bacteria naturally found in the lungs help create an environment that suppresses T-cell activation in the lymph nodes near the lungs. Conversely, that kind of immune-suppressive environment wasn’t found in lymph nodes near tumors growing near the animals’ skin. The investigators hope that their findings could help lead to the development of new ways to boost the immune response to lung tumors.
“There is a functional difference between the T-cell responses that are mounted in the different lymph nodes,” said Stefani Spranger, PhD, the Howard S. and Linda B. Stern career development assistant professor of biology, a member of MIT’s Koch Institute for Integrative Cancer Research, and senior author of the team’s paper, which is published in Immunity. “We’re hoping to identify a way to counteract that suppressive response so that we can reactivate the lung-tumor-targeting T cells.” Spranger, together with lead author, Maria Zagorulya, and colleagues, described their findings in a report titled “Tissue-specific abundance of interferon-gamma drives regulatory T cells to restrain DC1-mediated priming of cytotoxic T cells against lung cancer,” in which they concluded, “An improved mechanistic understanding of peripheral tolerance regulation could inspire new therapeutic approaches to disrupt immune tolerance against cancer and boost protective antitumor immunity.”
For many years, scientists have known that cancer cells can send out immunosuppressive signals, which leads to a phenomenon known as T-cell exhaustion. Cancer immunotherapy is designed to rejuvenate those T cells so that they can begin attacking tumors again. One type of immunotherapy involves the use of checkpoint inhibitors, which remove the brakes on exhausted T cells and help to reactivate them. This approach has worked well with cancers such as melanoma, but not as well with lung cancer.
Spranger’s recent work has offered one possible explanation for this. Her team found that some T cells stop working even before they reach a tumor, because of a failure to become activated early in their development. “In lung cancer, priming induces a T-cell dysfunction program that prevents CTL [cytotoxic T lymphocyte] differentiation and drives resistance to immune checkpoint blockade (ICB) therapy,” the authors wrote. “Hence, DC1-derived signals available during priming are instrumental for shaping the quality of the anti-tumor T-cell response.” In prior work, Spranger identified populations of dysfunctional T cells that can be distinguished from normal T cells by a pattern of gene expression that prevents them from attacking cancer cells when they enter a tumor. Despite the fact that these T cells are proliferating, and they’re infiltrating the tumor, they were never licensed to kill,” Spranger explained.
However, how tissue-specific immunoregulatory mechanisms influence anti-tumor T-cell responses remains poorly understood. The researchers delved further into this activation failure, which occurs in the lymph nodes. “In this study, we sought to uncover lung cancer-specific mechanisms driving dysfunctional tumor-reactive CD8+ T cells during T-cell priming,” the investigators stated. Lymph nodes filter fluids that drain from nearby tissues, and are also where killer T cells encounter dendritic cells that present the tumor antigens, and help to activate the T cells. “Cytotoxic CD8+ T cells are essential for anti-tumor immunity, and naive CD8+ T cells acquire cytotoxic function following priming by type 1 conventional dendritic cells (DC1s) in the tumor-draining lymph nodes,” the team further explained.
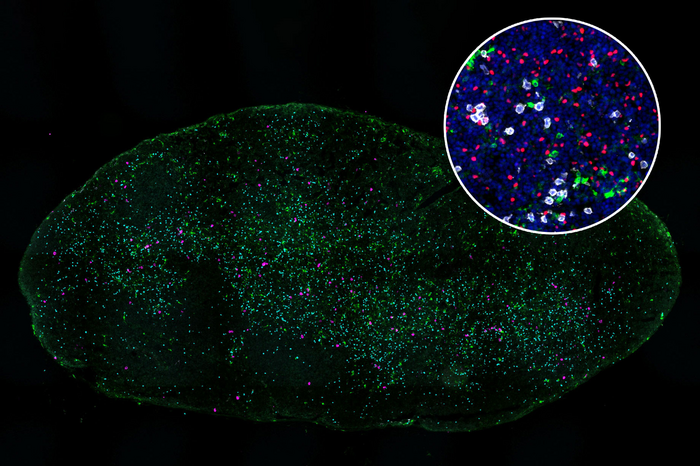
To explore why some killer T cells fail to be properly activated, Spranger’s team studied mice that had tumors implanted either in the lungs or in the flank. All of the tumors were genetically identical. The researchers found that T cells in lymph nodes that drain from the lung tumors did encounter type 1 conventional dendritic cells and recognize the tumor antigens displayed by those cells. However, these T cells failed to become fully activated, as a result of inhibition by another population of TH1-type regulatory T cells.
These regulatory T cells became strongly activated in lymph nodes that drain from the lungs, but not in tumor-draining lymph nodes near tumors located in the flank, the researchers found. Regulatory T cells are normally responsible for making sure that the immune system doesn’t attack the body’s own cells. However, the researchers found that these T cells also interfere with dendritic cells’ ability to activate killer T cells that target lung tumors. “By comparing T-cell responses in the mediastinal (mLN) and inguinal (iLN) LN that drained lung and flank tumors, respectively, we determined that Treg cells in the mLN restrained DC1-mediated priming of CTLs more effectively than their counterparts in the iLN,” Spranger et al., noted.
The researchers also discovered that these regulatory T cells suppress dendritic cells by removing stimulatory proteins from the surface of dendritic cells, which prevents them from being able to turn on killer T-cell activity. “Mechanistically, Treg cells in the tumor-draining mLN suppressed DC1 stimulatory signals needed to drive successful CTL differentiation.”
Further studies revealed that the activation of regulatory T cells is driven by high levels of interferon gamma (IFN-γ) in the lymph nodes that drain from the lungs. “Suppressive, clonally expanded TH1-like Treg cells were preferentially induced in the mLN in response to the tissue-specific abundance of interferon gamma (IFN-γ),” the team noted … Indeed, IFN-γ was 3.78-fold more enriched in the tumor-draining mLN compared with the iLN.”
The interferon gamma is produced in response to the presence of commensal bacterial—bacteria that normally live in the lungs without causing infection. “We found that TH1-like eTreg cell responses in the lung setting were driven by the mLN-specific abundance in IFN-γ, which was induced by commensal bacteria,” they wrote. “Consistent with our findings, the lung microbiome can directly impact lung-specific immunoregulatory mechanisms as well as anti-tumor immunity … The microbiome has further been reported to regulate the suppression capacity and frequency of Treg cells.”
The researchers have not yet identified the types of bacteria that induce this response or the cells that produce the interferon gamma, but they showed that when treating mice using an antibody that blocks interferon gamma restored killer T-cell activity. “Antibody-mediated IFN-γ blockade could counter the naturally increased IFN-γ abundance in the mLN, resulting in Treg cell repolarization and enhanced CTL responses against lung tumors.”
Interferon gamma has a variety of effects on immune signaling. Blocking it can dampen the overall immune response against a tumor, so using this strategy to stimulate killer T cells would not be a good strategy to use in patients, Spranger said. Her lab is now exploring other ways to help stimulate the killer T-cell response, such as inhibiting the regulatory T cells that suppress the killer T-cell response or blocking the signals from the commensal bacteria, once the researchers identify them. “Further research is needed to discern additional stimuli that regulate peripheral tolerance at different anatomic sites,” the authors further stated.