Getting a diagnosis is often, at the very least, a positive step toward selecting an appropriate treatment plan. However, the diagnosis of pancreatitis can often be met with the same abject feelings as no diagnosis at all, as the triggers for the disease have remained enigmatic. This has led to difficulties in developing efficacious therapeutics to treat chronic versions of the disorder. Patients suffering from chronic pancreatitis experience either recurring or permanent inflammation of their pancreas, but many anti-inflammatory agents are ineffective. Now, investigators at the Technical University of Munich (TUM) may have finally uncovered the underlying mechanism behind this inflammatory event.
Previous research was focused on the so-called acinus cells of the pancreas, as these are responsible for creating digestive enzymes. Many patients suffering from genetically caused pancreatitis show mutations in digestive enzymes or in molecules inhibiting the enzymes’ effectiveness.
“In many cases, people develop this disease because they are drinking too much alcohol, or they are smoking too much. Certain medication or high levels of lipids or calcium in a patient’s blood can be another cause of pancreatitis,” explained co-senior study investigator Heiko Witt, PhD, professor for pediatric nutritional medicine at the Else Kröner-Fresenius-Zentrum (EKFZ) at TUM.
Findings from the new study were published recently in Gastroenterology through an article titled, “Variants That Affect Function of Calcium Channel TRPV6 Are Associated With Early-Onset Chronic Pancreatitis.”
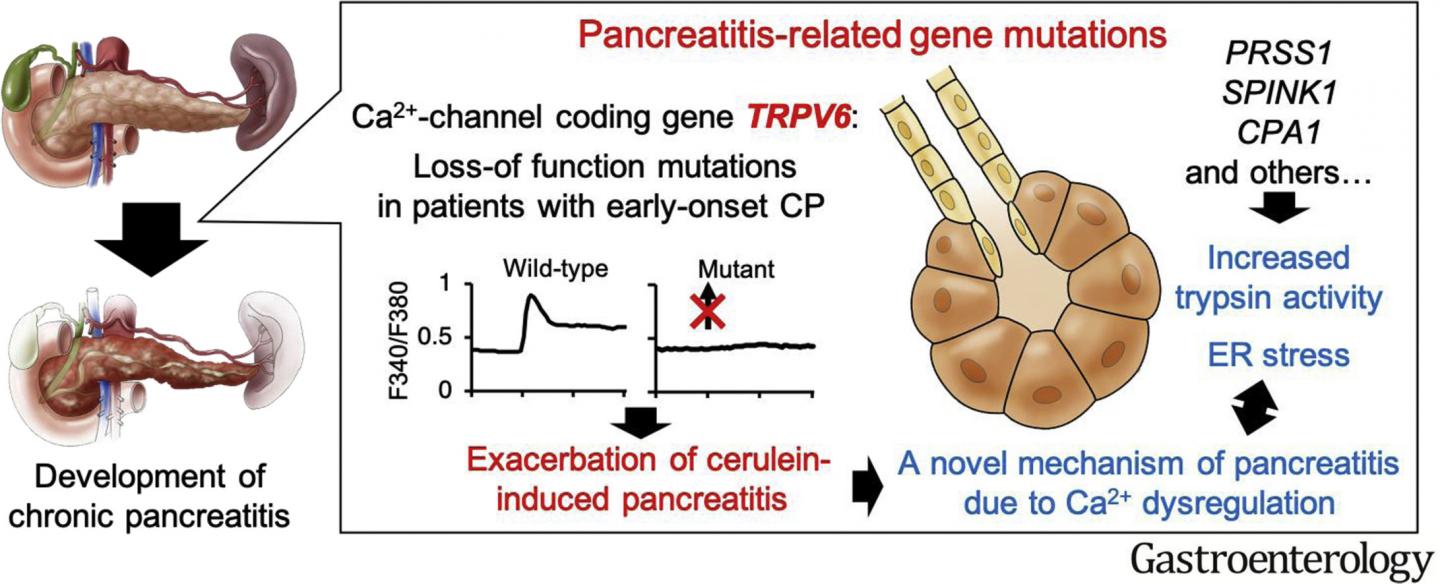
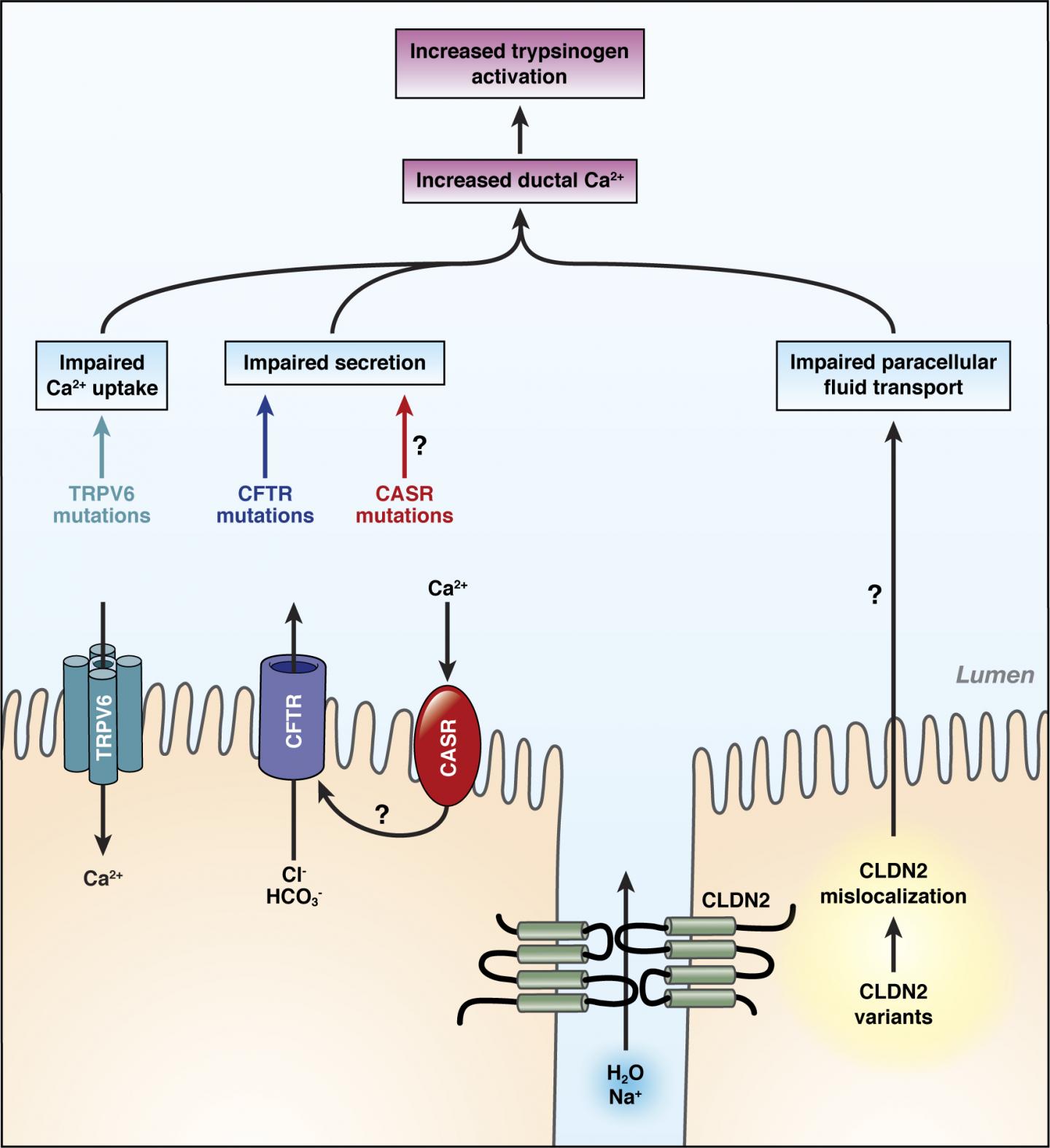
“A substantial TRPV6 defect is a globally occurring and serious risk factor for developing chronic pancreatitis,” noted Witt. “By identifying alterations of the calcium channel, we are now also considering duct cells as part of the concept covering the origins of this disease.” Duct cells serve as a coating in the channels that transport digestive enzymes from the point of origin into the intestines.
“We performed whole-exome DNA sequencing from a patient with idiopathic chronic pancreatitis (CP) and from his parents, who did not have CP,” the authors wrote. “We validated our findings by sequencing DNA from 300 patients with CP (not associated with alcohol consumption) and 1,070 persons from the general population in Japan (control individuals). In replication studies, we sequenced DNA from patients with early-onset CP (20 years or younger) not associated with alcohol consumption from France (n = 470) and Germany (n = 410). We expressed TRPV6 variants in HEK293 cells and measured their activity using Ca2+ imaging assays. CP was induced by repeated injections of cerulein in TRPV6mut/mut mice.”
The discovery that a calcium channel malfunction can contribute to the development of pancreatitis offers a new course of action for therapeutic intervention. Furthermore, the research findings will become part of the standard diagnostics for genetically caused pancreatitis.
These insights also pave the way for a new area of research covering the investigation of causes of pancreatitis—no longer focused on acinus cells and digestive enzymes but rather on duct cells and channels as well as calcium metabolism.
The identification of mutations in a calcium channel as a (contributing) cause of disease leads to new factors—other calcium channels and proteins that are relevant for calcium metabolism—moving into the scientific focus.
“Currently we are investigating these genes for genetic alterations and we have a European patient collective comprising 1,100 people with pancreatitis to gather our data,” Witt concluded. “Deciphering the genetic backgrounds of pancreatitis will substantially affect our understanding of these types of genetically caused pancreatitis, as well as our understanding of alcohol-related pancreatitis. It will enable new research approaches which may lead to new treatment possibilities in the future.”







