A promising new approach to potentially treating, and vaccinating against Alzheimer’s disease has been developed by researchers at the University of Leicester, the University Medical Center, Göttingen, and the medical research charity LifeArc. Rather than focus on the amyloid beta (Aβ) protein plaques in the brain—which are commonly associated with Alzheimer’s disease—the antibody and vaccine both target a different, soluble form of the protein, which is thought to be highly toxic. The team’s studies, reported in Molecular Psychiatry, showed that both the antibody-based treatment and the protein-based vaccine reduced Alzheimer’s symptoms in mouse models of the disease.
The researchers, headed Thomas Bayer, PhD, from the University Medical Center Göttingen, described their work in a paper titled, “Discovery of a novel pseudo β-hairpin structure of N-truncated amyloid-β for use as a vaccine against Alzheimer’s disease,” in which they wrote, “Here we report the discovery of a unique conformational epitope in the N-terminal region of Aβ, which offers new routes for active and passive immunization against AD… we have developed a novel AD vaccine with unique features not related to any other vaccine or antibody in clinical development.” The investigators are also now looking to find a commercial partner to take the therapeutic antibody and the vaccine through clinical trials.
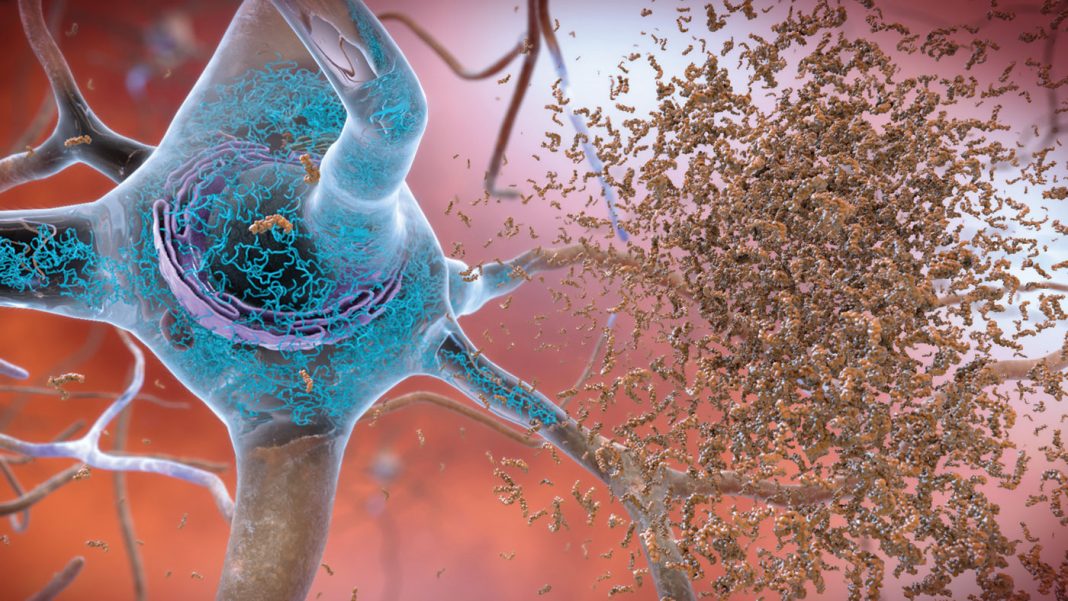
One of the hallmarks of Alzheimer’s disease is deposits of amyloid beta protein in amyloid plaques in the brain, the authors noted. Amyloid beta protein naturally exists as highly flexible, string-like molecules in solution, which can join together to form fibers and plaques. In Alzheimer’s disease, a high proportion of these string-like molecules become shortened—truncated—and some scientists now think that these forms are key to development and progression of the disease. “The Aβ peptide exists in several forms, including full-length Aβ1-42 and Aβ1-40—and the N-truncated species, pyroglutamate Aβ3-42 and Aβ4-42, which appear to play a major role in neurodegeneration,” the investigators stated.
The team had previously identified a murine antibody (TAP01), which binds specifically to soluble, non-plaque N-truncated Aβ species. Preeti Bakrania, PhD, and colleagues from LifeArc adapted this antibody so the human immune system wouldn’t recognize it as foreign, and would accept it. Bayer noted, “In clinical trials, none of the potential treatments which dissolve amyloid plaques in the brain have shown much success in terms of reducing Alzheimer’s symptoms. Some have even shown negative side effects. So, we decided on a different approach. We identified an antibody in mice that would neutralize the truncated forms of soluble amyloid beta, but would not bind either to normal forms of the protein or to the plaques.”
When the Leicester research group looked at how and where this ‘humanized’ antibody, called TAP01_04, was binding to the truncated form of amyloid beta, the team had a surprise. They saw the amyloid beta protein was folded back on itself, in a hairpin-shaped structure. “… we report that TAP01 family antibodies uniquely bind to a novel, pseudo β-hairpin conformation of the N-terminal region of Aβ, which is not related to any other Aβ epitope, conformation, or aggregate structure described so far.”
Mark Carr, PhD, from the Leicester Institute of Structural and Chemical Biology at the University of Leicester, further explained, “This structure had never been seen before in amyloid beta. However, discovering such a definite structure allowed the team to engineer this region of the protein to stabilize the hairpin shape and bind to the antibody in the same way. Our idea was that this engineered form of amyloid beta could potentially be used as a vaccine, to trigger someone’s immune system to make TAP01_04 type antibodies.”
When the team tested the engineered amyloid beta protein in vivo, they found that mice receiving the ‘vaccine’ did produce TAP01 type antibodies. The Göttingen group then tested both the humanized antibody and the engineered amyloid beta vaccine—the ‘TAPAS’ vaccine—in two different mouse models of Alzheimer’s disease. Based on similar imaging techniques to those used to diagnose Alzheimer’s in humans, they found that both the antibody and the vaccine helped to restore neuronal function, increase glucose metabolism in the brain, restore memory loss and—even though this wasn’t directly targeted—reduce amyloid beta plaque formation. “We engineered a stabilized cyclic form of Aβ1-14 (N-Truncated Amyloid Peptide AntibodieS; the TAPAS vaccine) … Active immunization of two mouse models of AD with the TAPAS vaccine led to a striking reduction in amyloid plaque formation, a rescue of brain glucose metabolism, a stabilization in neuron loss, and a rescue of memory deficiencies,” they wrote. “Treating both models with the humanized version of the TAP01 antibody had similar positive effects.”
Bakrania added, “The TAP01_04 humanized antibody and the TAPAS vaccine are very different to previous antibodies or vaccines for Alzheimer’s disease that have been tested in clinical trials because they target a different form of the protein. This makes them really promising as a potential treatment for the disease either as a therapeutic antibody or a vaccine. The results so far are very exciting and testament to the scientific expertise of the team. If the treatment does prove successful, it could transform the lives of many patients.”
Carr further stated, “While the science is currently still at an early stage, if these results were to be replicated in human clinical trials, then it could be transformative. It opens up the possibility to not only treat Alzheimer’s once symptoms are detected, but also to potentially vaccinate against the disease before symptoms appear.”
As the authors concluded, “The novel TAPAS family of antibodies have revealed two new attractive options for therapeutic intervention in AD, with either active immunization using a cyclized peptide-based vaccine, or treatment with a humanized TAP01 family therapeutic antibody (passive immunization) … The positive therapeutic outcomes from active immunization with cyclic Aβ1-14 as well as the passive immunization with the clinical lead candidate antibody suggest the potential for a vaccine to protect future generations from this terrible disease.”