In science, the mantra “correlation does not equate causation” is a cornerstone of proper data analysis and hypothesis formation. Yet, for researchers, this code is not a stopping point, but often a springboard to dive more deeply into the data and discover the mechanisms that led to the curious findings. When the data is supported by a patient population of almost two million, it probably means you’re on to something that’s more than just a statistical artifact. This is most certainly the case for an interesting new finding by an international team of investigators led by scientists at the Van Andel Research Institute (VARI), which suggests that removing the appendix early in life reduces the risk of developing Parkinson’s disease by 19–25%.
The findings from this comprehensive study were released through an article published in Science Translational Medicine titled “The vermiform appendix impacts the risk of developing Parkinson’s disease.” This data solidifies the role of the gut and immune system in the genesis of the disease and reveals that the appendix acts as a major reservoir for abnormally folded α-synuclein proteins, which are closely linked to Parkinson’s onset and progression.
“Our results point to the appendix as a site of origin for Parkinson’s and provide a path forward for devising new treatment strategies that leverage the gastrointestinal tract’s role in the development of the disease,” explained senior study investigator Viviane Labrie, Ph.D., an assistant professor at VARI. “Despite having a reputation as largely unnecessary, the appendix actually plays a major part in our immune systems, in regulating the makeup of our gut bacteria and now, as shown by our work, in Parkinson’s disease.”
Interestingly, the reduced risk for Parkinson’s was only apparent when the appendix, and the α-synuclein contained within it, were removed early in life, years before the onset of Parkinson’s, suggesting that the appendix may be involved in disease initiation. Removal of the appendix after the disease process starts, however, had no effect on disease progression.
“We determined the capacity of the appendix to modify PD risk and influence pathogenesis,” the authors wrote. “In two independent epidemiological datasets, involving more than 1.6 million individuals and over 91 million person-years, we observed that removal of the appendix decades before PD onset was associated with a lower risk for PD, particularly for individuals living in rural areas, and delayed the age of PD onset.”
The research team also found that appendectomy can delay disease progression in people who go on to develop Parkinson’s, pushing back diagnosis by an average of 3.6 years. Because there are no definitive tests for Parkinson’s, people often are diagnosed after motor symptoms such as tremor or rigidity arise. By then, the disease typically is quite advanced, with significant damage to the area of the brain that regulates voluntary movement.
Conversely, appendectomies had no apparent benefit in people whose disease was linked to genetic mutations passed down through their families, a group that comprises fewer than 10% of cases.
“Our findings today add a new layer to our understanding of this incredibly complex disease,” noted lead study investigator Bryan Killinger, Ph.D., a postdoctoral fellow in Dr. Labrie’s laboratory. “We have shown that the appendix is a hub for the accumulation of clumped forms of α-synuclein proteins, which are implicated in Parkinson’s disease. This knowledge will be invaluable as we explore new prevention and treatment strategies.”
Amazingly, the researchers also found clumps of α-synuclein in the appendixes of healthy people of all ages as well as people with Parkinson’s, raising new questions about the mechanisms that give rise to the disease and propel its progression. Clumped α-synuclein is considered to be a key hallmark of Parkinson’s—previously, it was thought to only be present in people with the disease.
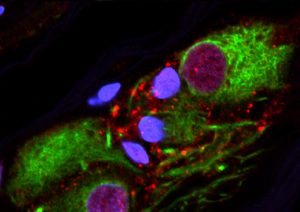
“We also found that the healthy human appendix contained intraneuronal α-synuclein aggregates and an abundance of PD pathology–associated α-synuclein truncation products that are known to accumulate in Lewy bodies, the pathological hallmark of PD,” the authors penned. “Lysates of human appendix tissue induced the rapid cleavage and oligomerization of full-length recombinant α-synuclein.”
Data for the study were gleaned from an in-depth characterization and visualization of α-synuclein forms in the appendix, which bore a remarkable resemblance to those found in the Parkinson’s disease brain, as well as analyses of two large health-record databases. The first dataset was garnered from the Swedish National Patient Registry, a one-of-a-kind database that contains de-identified medical diagnoses and surgical histories for the Swedish population beginning in 1964, and Statistics Sweden. The team at VARI collaborated with researchers at Lund University, Sweden, to comb through records for 1,698,000 people followed up to 52 years, a total of nearly 92 million person-years. The second dataset was from the Parkinson’s Progression Marker Initiative, which includes details about patient diagnosis, age of onset, demographics, and genetic information.
“We were surprised that pathogenic forms of α-synuclein were so pervasive in the appendixes of people both with and without Parkinson’s. It appears that these aggregates—although toxic when in the brain—are quite normal when in the appendix. This clearly suggests their presence alone cannot be the cause of the disease,” Dr. Labrie concluded. “Parkinson’s is relatively rare—less than 1% of the population—so there must be some other mechanism or confluence of events that allows the appendix to affect Parkinson’s risk. That’s what we plan to look at next—which factor or factors tip the scale in favor of Parkinson’s?”







