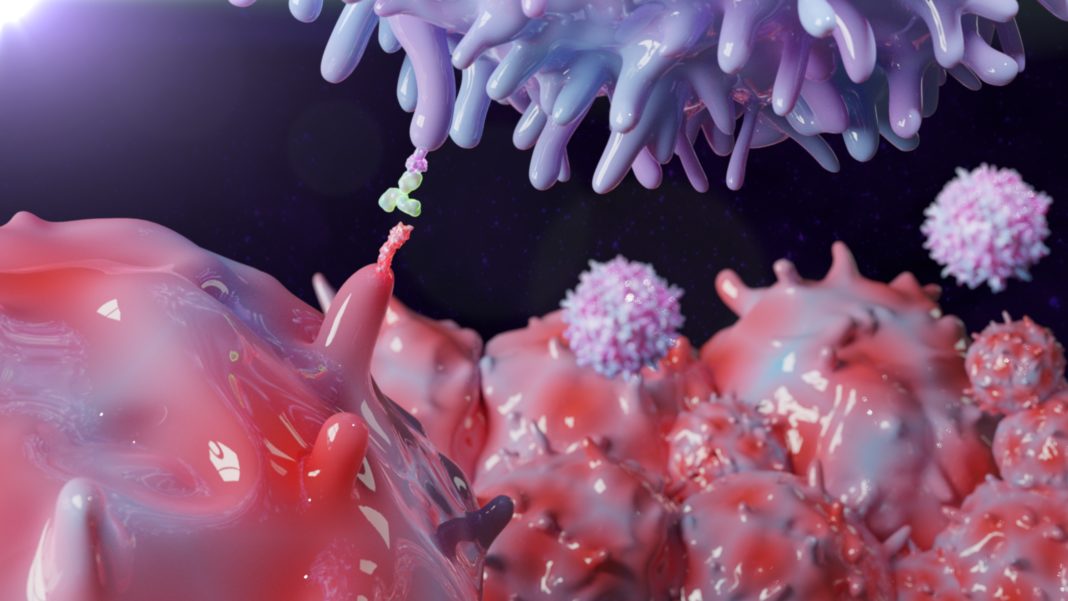
Immune checkpoint inhibitors (ICIs), drugs that release the immune system’s “brakes,” are meant to expose cancer to the full force of the immune system’s attack. But in most cancer patients, ICIs leave the brakes engaged. To understand why this is the case—and to identify ways that ICIs could succeed more often—scientists based at Columbia University and the Massachusetts Institute of Technology have created a new technique to study ICI resistance (ICR).
Essentially, the technique, which is called Perturb-CITE-sequencing (or Perturb-CITE-seq), surveys the pathways that cancer cells may use to escape ICI immunotherapy. Perturb-CITE-seq is an extension of Perturb-seq, a technique that combines CRISPR-based perturbation screens and massively parallel single-cell RNA sequencing. Like Perturb-seq, Perturb-CITE-seq provides RNA readouts. In addition, however, Perturb-CITE-seq provides protein readouts, that is, information about the epitopes (antibody-binding sites) of cell surface proteins. (CITE-seq stands for cellular indexing of transcriptomes and epitopes by sequencing.)
To show what Perturb-CITE-seq can do, the Columbia/MIT team tested it with cancer cells and matching immune cells, tumor-infiltrating lymphocytes (TILs), from melanoma patients. Specifically, the scientists performed pooled Perturb-CITE-seq screens of ICR program genes in a unique patient-derived malignant-TIL co-culture model, targeting 248 genes with a putative role in ICR (744 targeting guides) and profiling single-cell transcriptomes and 20 surface proteins in >218,000 cells. Doing so allowed the scientists to identify previously unknown ICR mechanisms—mechanisms that may explain why ICIs fail or stop working in two-thirds of melanoma patients.
Details of this work appeared March 1 in Nature Genetics, in an article titled, “Multimodal pooled Perturb-CITE-seq screens in patient models define mechanisms of cancer immune evasion.” The article describes what Perturb-CITE-seq revealed when it was applied to dissect critical interactions at the tumor-immune synapse.
“We recover known mechanisms of resistance, including defects in the interferon-γ (IFN-γ)–JAK/STAT and antigen-presentation pathways in RNA, protein, and perturbation space, and new ones, including loss/downregulation of CD58,” the article’s authors wrote. “Loss of CD58 conferred immune evasion in multiple co-culture models and was downregulated in tumors of melanoma patients with ICR. CD58 protein expression was not induced by IFN-γ signaling, and CD58 loss conferred immune evasion without compromising major histocompatibility complex (MHC) expression, suggesting that it acts orthogonally to known mechanisms of ICR.”
“With ICIs, we’re now getting as close as we have ever been to curing one-third of patients with metastatic melanoma, even at a stage when the disease has spread throughout the body,” said the article’s co-corresponding author, Benjamin Izar, MD, PhD, assistant professor of medicine at Columbia University Vagelos College of Physicians and Surgeons. “So, the question is, what is happening in the other two-thirds of patients? What are the mechanisms of intrinsic or adaptive drug resistance?”
In a previous study published in Cell in 2018, Izar and his team identified 248 genes in metastatic melanoma cells that allow them to evade ICIs. The new study was devised to provide a systematic way to functionally decipher how each of those genes contributes to immunotherapy resistance.
With their Perturb-CITE-seq system, the scientists used CRISPR to inactivate those 248 genes—one by one but in a pooled fashion—to create a mixture of 248 batches of melanoma cells, each with a different mutation. The entire heterogenous population of “edited” cancer cells was then exposed to T cells—the TILs unleashed by ICIs in patients.
Cells that resisted being killed by T cells were isolated, and a snapshot of all active processes within these cells was measured using single-cell RNA and protein profiling, providing a high-resolution molecular map of several gene perturbations resulting in immune escape.
“Our approach is unique in that we study these mechanisms in patient-derived models,” Izar declared. “Rather than looking at how a gene changes a cell’s phenotype one gene at a time, we were able to study many genes with potential roles in drug resistance in patients in one sweep. It’s the first time that such tools have been used at such a large scale.”
All told, close to a quarter million cells were analyzed. Computational biology tools, developed by Izar and co-corresponding author Aviv Regev, PhD, professor of biology at MIT, were employed to make sense of this tremendous data set.
The analysis identified new mechanisms of resistance to immunotherapy along with mechanisms that were previously known. “Basically, we recovered the majority of known mechanisms described over the last 10 years—validating that our approach works and giving us confidence that the new findings are important,” Izar noted.
“We also uncovered many new mechanisms of resistance,” said Johannes C. Melms, MD, a postdoctoral fellow in the Izar lab and the study’s co-first author (with Chris J. Frangieh, a doctoral student at MIT).
One of the new resistance mechanisms involves a gene called CD58. “Our data suggests that loss of CD58 in melanoma cells confers immune escape through three potential mechanisms: impairing activation of T cells, reducing the ability of T cells getting into the tumor, and increasing the production of PD-L1,” Melms detailed. “Because the CD58 gene is not mutated per se but rather just turned off, it raises the possibility that therapies that turn it on could overcome drug resistance in some patients.”
The researchers plan to develop therapies to improve response to immunotherapies based on this finding.
Izar and his team expect to learn more about resistance to immunotherapy from the study data. “CD58 is just one of many genes that warrant a closer look,” Izar observed. In future experiments, the researchers plan to inactivate various combinations of cancer cell genes at once.
“In this study, we looked at what happens to cells when only one gene is inactivated,” Izar emphasized. “But it’s likely that no single gene is sufficient to confer all the types of resistance to immunotherapy that we see in clinical practice.”
The study focused on melanoma, but the same approach could be used to study resistance to immunotherapy in many other forms of cancer, the researchers noted.