For women who are carriers of mitochondrial diseases, one particular in vitro fertilization (IVF) procedure for having a healthy baby appears to be safe, according to new research.
This option, called “spindle transfer,” involves transferring the nuclear DNA from one of the woman’s eggs into an enucleated donor egg that contains healthy mitochondria before being fertilized with sperm from a male partner. The new research uses single-cell multiomics techniques to show that this option results in embryos that are comparable to healthy controls produced by standard IVF techniques.
The work, published in PLoS Biology (“Single-cell multiomics analyses of spindle-transferred human embryos suggest a mostly normal embryonic development”), was led by Wei Shang, a physician at Chinese PLA General Hospital, Beijing, and Fuchou Tang, PhD, of Peking University, Beijing.
Mitochondria with certain DNA mutations can cause a variety of metabolic, muscular, and neurologic disorders. In human reproduction, only the maternal mitochondria, contained in the egg, are inherited. The results from the new study are likely to spur further adoption of spindle transfer for IVF when there is a risk of mitochondrial disease.
“Mitochondrial DNA (mtDNA) mutations are often associated with incurable diseases and lead to detectable pathogenic variants in 1 out of 200 babies,” explained the researchers in their paper.
“Uncoupling of the inheritance of mtDNA and the nuclear genome by spindle transfer (ST) can potentially prevent the transmission of mtDNA mutations from mother to offspring,” they continued. The “spindle” refers to the apparatus that holds the chromosomes in place.
Spindle transfer has been used clinically, but questions remain about its safety. Until now, no systematic omics study had been implemented on the spindle transfer procedure in human embryos.
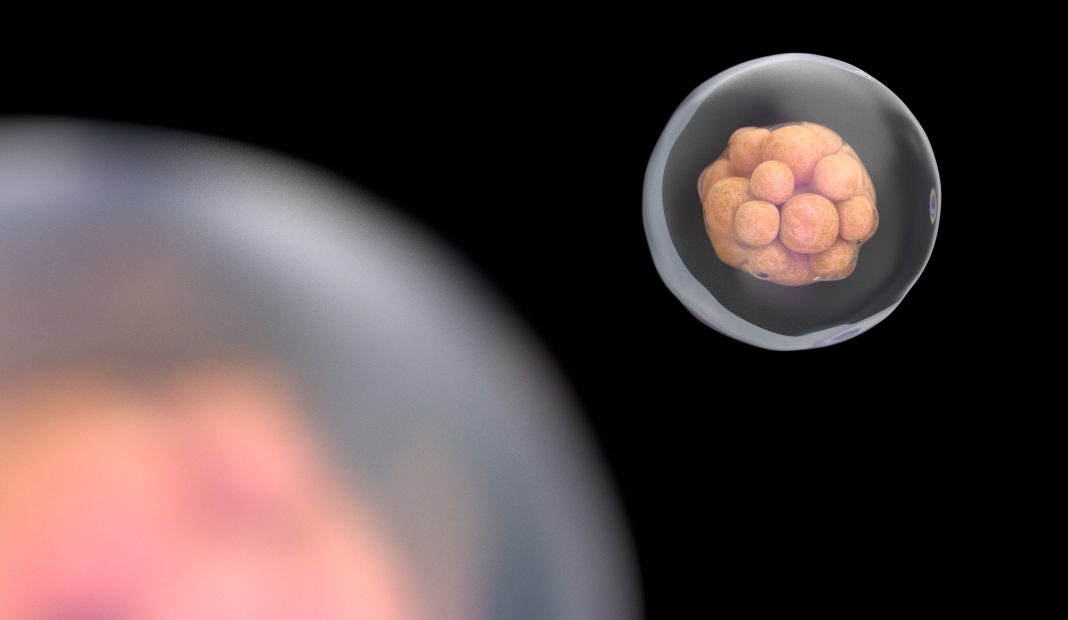
The researchers analyzed single cells from blastocysts—balls of cells that form after fertilization. “The blastocyst stage is the last in vitro developmental stage of the assisted reproductive technology (in vitro fertilization and embryo transfer) [which is why] we chose human blastocysts to do single-cell multiomics analyses,” the researchers wrote.
They compared cells from 23 blastocysts that formed following spindle transfer to cells from 23 control IVF blastocysts and found no difference in DNA copy number (a measure of genomic integrity) or RNA expression profiles.
However, they did find a small but significant reduction in the level of DNA demethylation in spindle transfer blastocysts in one layer, the trophectoderm, though not in two other layers. DNA demethylation is one of the processes used to increase gene expression during development.
The reduction may be evidence of a slight delay in the process, rather than a permanent inability to upregulate the affected genes. “It is quite possible that after the blastocyst stage, the spindle transfer embryos can catch up to complete DNA demethylation before implantation [in the uterine wall],” Tang said.
But the scope of the work was somewhat limited. In the future, more embryos, more developmental stages, and more aspects of embryo biology should be studied, they point out.
“One of the key factors driving ST to the clinic is safety,” the researchers wrote. “[Our] work provides the first comprehensive set of molecular evidence indicating that ST seems generally safe in human embryos and deserves further rigorous scientific evaluations and even clinical testing.”