HIV controllers, the rare individuals who can control HIV naturally, have a secret—or rather their killer T cells do. These cells are energy omnivores. That is, they are not heavily dependent on glucose, like the killer T cells from noncontrollers. They may draw on varied metabolic resources. This flexibility, this metabolic plasticity, gives killer T cells from controllers exceptional staying power when fighting HIV. And now, as demonstrated by scientists at the Institut Pasteur, this metabolic plasticity can be programmed into killer T cells from noncontrollers.
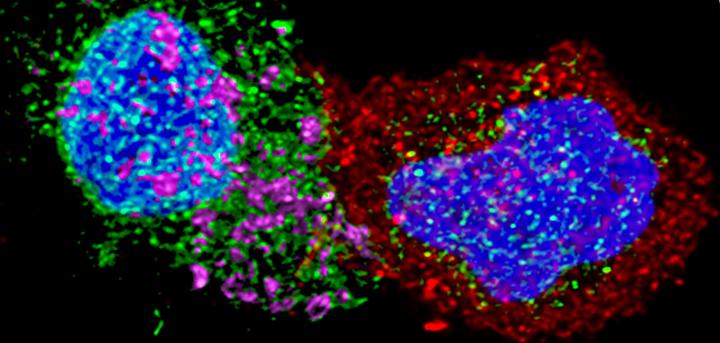
Back in 2007, Institut Pasteur scientists described the extraordinary antiviral activity of killer T cells, or CD8+ lymphocytes, taken from HIV controllers. Unlike the CD8+ cells of noncontrollers, the CD8+ cells of HIV controllers can rapidly destroy infected CD4+ cells.
Extending this research, scientists from the Institut Pasteur’s HIV, Inflammation and Persistence Unit investigated the specific characteristics of these cells. The scientists determined that the unique antiviral power of these immune cells can be attributed to an optimal metabolic program that confers persistence and the ability to react effectively against infected cells. Then, working ex vivo, the scientists successfully reprogrammed cells from infected noncontroller individuals to give them the same antiviral potency as controllers’ cells.
Details of this new work appeared July 12 in the journal Nature Metabolism, in an article entitled, “Metabolic plasticity of HIV-specific CD8+ T cells is associated with enhanced antiviral potential and natural control of HIV-1 infection.” The article describes how single-cell analysis was used to show that HIV-specific, central memory CD8+ T cells from spontaneous HIV controllers and anti-retrovirally treated noncontrollers have opposing transcriptomic profiles.
“Genes linked to effector functions and survival are upregulated in cells from HIV controllers,” the article’s authors indicated. “In contrast, genes associated with activation, exhaustion, and glycolysis are upregulated in cells from noncontrollers.”
Outwardly, the CD8+ T cells of controllers appear to be identical to those of noncontrollers. But controllers and noncontrollers have CD8+ T cells that follow different molecular programs. The anti-HIV CD8 cells in controllers not only have huge antiviral potential, they are also programmed to survive, whereas in noncontrollers, the cell program predisposes them to exhaustion and cell death.
“HIV-specific CD8+ T cells from noncontrollers are largely glucose dependent, whereas those from HIV controllers have more diverse metabolic resources that enhance both their survival potential and their capacity to develop anti-HIV effector functions,” the current article emphasizes. “The functional efficiency of the HIV-specific CD8+ T cell response in HICs is thus engraved in their memory population and related to their metabolic program.”
In the laboratory, the scientists then managed to stimulate mitochondrial activity in the anti-HIV cells of noncontrollers. They used a substance secreted by the immune system known as interleukin 15 to boost the mitochondrial activity of noncontrollers’ cells and increase their anti-HIV potential. The reprogrammed CD8+ T cells of noncontrollers are able to destroy infected CD4+ T cells, much like controllers’ cells.
“We identified that the antiviral activity of CD8+ T cells in controllers is associated with an optimal program that gives them plasticity in using the cell’s energy resources,” said the Institut Pasteur’s Asier Sáez-Cirión, PhD, the senior author of the current study. “Our research shows that even if the anti-HIV CD8+ cells of noncontrollers are relatively ineffective compared with those of controllers, the differences can be overcome.”