Researchers from the group of Jeroen Bakkers, PhD, at the Hubrecht Institute, have shed new light on the remarkable capacity of the zebrafish to recover from cardiac damage and regenerate functional heart cells. The team’s reported study uncovered a new mechanism that functions as a switch to push the heart muscle cells, or cardiomyocytes, to mature in the regeneration process. Importantly, the findings suggest that this mechanism is conserved, as it exhibited a very similar effect on mouse and human heart muscle cells.
The researchers said their study demonstrates how examining the natural heart regeneration process in zebrafish and applying these discoveries to human heart muscle cells could contribute to the development of new therapies against cardiovascular diseases.
Bakkers and colleagues reported on the work in Science, in a paper titled “Interplay between calcium and sarcomeres directs cardiomyocyte maturation during regeneration.” In their paper the team concluded “This study provides evidence that rather than being a passive event, CM maturation is an active process.”
The human heart has only limited self-healing capacity, and cardiovascular diseases, including heart attacks—or myocardial infarction—result in an estimated 18 million deaths every year, according to the researchers. After a myocardial infarction (MI), the mammalian heart loses millions of cardiomyocytes (CM), which are replaced by a permanent fibrotic scar. And although therapies exist that manage the symptoms of an MI, there is no treatment that is able to replace the lost tissue with functional, mature heart muscle cells.
Unlike humans, some species, such as the zebrafish, can regenerate their hearts. The surviving heart muscle cells are able to divide and produce more cells. This unique feature provides zebrafish hearts with a source of new tissue to replace the lost heart muscle cells, and means that about 90 days after damage to its heart has occurred, the animal can have achieved fully restored its cardiac function.
Previous studies have identified factors that could stimulate heart muscle cells to divide. However, as the authors noted, what happens to the newly formed heart muscle cells afterwards had not been studied before. “However, little is known about the mechanisms that restore the injured heart to its original size and function … Although the steps leading up to the proliferation of surviving cardiomyocytes have been extensively studied, little is known about the mechanisms that control proliferation and redifferentiation to a mature state.”
Phong Nguyen, PhD, first author of the newly reported study, explained, “It is unclear how these cells stop dividing and mature enough so that can they contribute to normal heart function. We were puzzled by the fact that in zebrafish hearts, the newly formed tissue naturally matured and integrated into the existing heart tissue without any problems.”
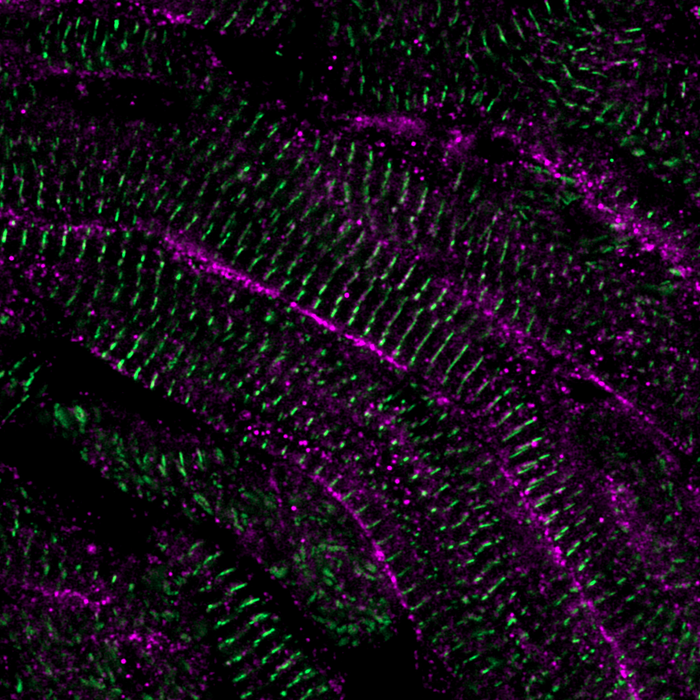
To study maturation of the newly formed tissue in detail, the researchers developed a technique that allowed them to culture thick slices of injured zebrafish hearts outside the body. This allowed them to perform live imaging on the movement of calcium in heart muscle cells. The regulation of calcium moving in and out of heart muscle cells is important for controlling heart contractions and can predict the maturity of the cell. AS they explained, “Because Ca2+ handling changes as CMs mature, we developed an ex vivo imaging system using a transgenic zebrafish line that expressed the fluorescent Ca2+ sensor GCaMP6f specifically in CMs to track the dynamics during regeneration.”
Their results showed that after the heart muscle cells divide, calcium movements changed over time. “The calcium movement in the newly divided cell was initially very similar to embryonic heart muscle cells, but over time the heart muscle cells assumed a mature type of calcium movement,” Nguyen said. “We found that the cardiac dyad, a structure that helped to move calcium within the heart muscle cell, and specifically one of its components, LRRC10, was crucial in deciding whether heart muscle cells divide or progress through maturation. Heart muscle cells that lack LRRC10 continued to divide and remained immature.” Reporting in their paper on their findings, the investigators stated, “Lrrc10 plays a critical role in actively maturing CMs by inhibiting early regeneration hallmarks, whereas lrrc10 mutants appeared to be perpetually held in an early regeneration phase and consequently failed to regenerate.”
After the researchers established the importance of LRRC10 in stopping cell division and initiating maturation of zebrafish heart muscle cells, they moved on to test if their findings could be translated to mammals. To this end, they induced the expression of LRRC10 in mouse and lab-grown human heart muscle cells (human induced pluripotent stem cell CMs; hiPSC-CMs). Strikingly, LRRC10 changed calcium handling, reduced cell division and increased maturation of these cells in a similar manner to that observed in zebrafish hearts. Nguyen continued, “It was exciting to see that the lessons learned from the zebrafish were translatable as this opens new possibilities for the use of LRRC10 in the context of new therapies for patients”. Describing their results, the authors noted, “Overall, we found that the expression of LRRC10 is not associated with the end of maturation, but rather the onset of its expression appears to advance progression of hiPSC-CMs to a more mature state.”
The results of the study demonstrated that LRRC10 has the potential to drive the maturation of heart muscle cells further, through the control of their calcium handling. This could help scientists who are trying to solve the lack of regenerative capacity of the mammalian heart by transplanting lab-grown heart muscle cells into the damaged heart. Although this potential strategy has promise, results showed that these lab-grown cells are still immature and cannot communicate properly with the rest of the heart, leading to abnormal contractions called arrhythmias.
The investigators further noted, “Efficient communication between and within individual CMs permits synchronous contraction to produce maximum cardiac output. This remains an unresolved limiting factor for developing cellular-based therapies for heart failure.” Specifically, they noted, exogeneous cardiac tissue in which CM maturity has not been achieved precisely fails to integrate with the existing heart muscle, and so contraction is asynchronous, and “consequently, the long-term contribution to cardiac output is varied.”
“Although more research is needed to precisely define how mature these lab-grown heart muscle cells are when treated with LRRC10, it is possible that the increase in maturation will improve their integration after transplantation,” said Bakker. “Additionally, current models for cardiac diseases are frequently based on immature lab-grown heart muscle cells. 90% of promising drug candidates found in the lab fail to make it to the clinic and the immaturity of these cells could be one contributing factor for this low success rate. Our results indicate LRRC10 could improve the relevance of these models as well.”
LRRC10 could thus have an important contribution to generate lab-grown heart muscle cells that more accurately represent a typical adult human heart, therefore improving the chances of developing successful new treatments against cardiovascular diseases. The authos concluded, “This study shows the complex and highly interlinked interaction between sarcomere and Ca2+ regulation during CM maturation by using a cardiac regeneration model that naturally generates new CM … We showed that the cardiac dyad is vital for this maturation process, which may provide a potential target to promote CM maturation.”