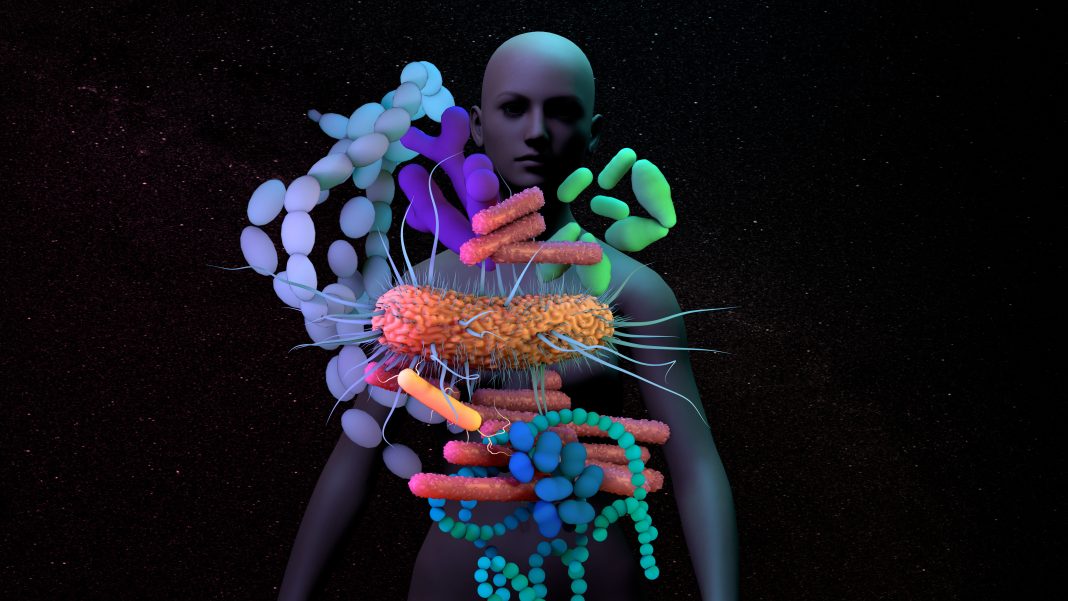
CAR-T cells are engineered cancer immunotherapies that boost or hijack a person’s immune system to target their cancer. Increasing evidence from human studies and preclinical experiments suggests that the gut microbiome may modulate the efficacy of T cell-driven cancer immunotherapies, such as immune checkpoint blockade. Now, researchers from German Cancer Research Center (DKFZ), together with colleagues from Germany, Israel, and the United States, have found that the gut microbiome may modulate the efficacy of CD19 CAR-T cell immunotherapy in patients with B cell leukemias and lymphomas.
The findings are published in Nature Medicine in a paper titled, “A non-antibiotic-disrupted gut microbiome is associated with clinical responses to CD19-CAR-T cell cancer immunotherapy.”
This largest prospective study of its kind has followed 172 lymphoma patients previously failing multiple rounds of chemotherapy, from before CAR-T immunotherapy initiation until two years later. Interestingly, 20% of patients receiving a subset of broad-spectrum (“high-risk”) antibiotics, such as meropenem, piperacillin–tazobactam, or cefepime, featured an altered clinical response to subsequent CAR-T therapy, compared to patients who received other antibiotics and patients who were not treated with antibiotics prior to therapy. However, this antibiotics-associated reduced CAR-T therapy response was not driven by the effects of the antibiotics themselves, but rather by the fact that patients treated with “high-risk” antibiotics before initiation of CAR-T therapy tended to have higher pre-therapy tumor burden and systemic inflammation as compared to non-antibiotics-treated patients. These adverse pre-treatment conditions rendered subsequent CAR-T therapy less effective.
The researchers identified several key microbiome features enabling the prediction of CAR-T efficacy, including species of Bacteroides, Ruminococcus, Eubacterium, and Akkermansia. Of these, Akkermansia was also associated with higher baseline peripheral T cell levels in these patients.
The study reveals strong associations between microbiomes and CAR-T outcomes. Additionally, findings from this study may lead to a better understanding of the differential CAR-T cell activation, persistence, and clinical efficacy in different patients. Eran Elinav, MD, PhD, director of the DKFZ-Weizmann Institute of Science Microbiome & Cancer Bridging division, concluded, “…With further research, we hope that microbiome-based diagnostics and therapies will be incorporated into the precision oncology field.”