Scientists at the Lewis Katz School of Medicine at Temple University (LKSOM) and the University of Pennsylvania have demonstrated how astrocytic glial cells in the brain can play a major role in facilitating neuron repair. The research, reported in Cell Metabolism, is the first to establish a link between glucose metabolism in glial cells and functional regeneration of damaged neurons in the central nervous system. “We found that glia have a metabolic switch associated with glucose metabolism that when triggered reverses inhibitory effects on growth and promotes axon regeneration,” commented Shuxin Li, MD, PhD, professor of anatomy and cell biology at Shriners Hospital’s Pediatric Research Center at LKSOM, and a senior investigator on the new study, which is titled, “Glial Metabolic Rewiring Promotes Axon Regeneration and Functional Recovery in the Central Nervous System.”
Dynamic networks that specialize in the transmission of information generally consist of multiple components, including not only primary processors, like computers, for example, but also numerous support applications and services. The human nervous system can be thought of as fundamentally very similar. Neurons, like computers, process and transmit information, sending molecular signals through axons to other neurons, all of which are supported by non-neuronal components, including an array of cells known as glia.
Nerve axons in the adult central nervous systems don’t regenerate if severely damaged, and the ability to prompt nerve regeneration after injury or as a result of disease, is a major goal for researchers working in the field. “Severed CNS axons fail to regenerate, resulting in permanent functional deficits in human patients, including SCI [spinal cord injury],” the scientists wrote. “Regarded as the holy grail in regenerative medicine, achieving axon regeneration and functional recovery in the central nervous system (CNS) after injury or in neurodegenerative diseases remains a daunting task.”
This inability of nerve axons in the CNS to regrow after injury is partly because of the “diminished intrinsic growth capacity of mature neurons,” the team continued, but is also because the CNS environment also inhibitory to axon regrowth, when compared with that of the more permissive peripheral nervous system.
Glial cells carry out a variety of support and maintenance functions, and one type in particular—the astrocytic glial cell—has the unique ability to form scar tissue around damaged neurons. The presence of scar tissue is associated with inhibitory effects on the regrowth of mature neurons that are damaged by spinal cord injury. However, recent evidence suggests that these inhibitory effects are reversible, and the work now reported by Li and collaborating scientists indicates how astrocytic glial cells may play a part in enabling neuron repair.
In collaboration with senior investigator Yuanquan Song, PhD, Assistant Professor of Pathology and Laboratory Medicine at the University of Pennsylvania Perelman School of Medicine, Li and colleagues set out to investigate how scar tissue formation induced by glial cells impacts axon regeneration, using both fly and mouse models of axon injury. “ … in this study, we asked if, by approaching a specific status of glial cells, the inhibitory CNS environment can be reversed to support axon regeneration,” they wrote. In initial experiments, the team confirmed that, as previous studies had indicated, the negative effects of glial cell activity on axon regeneration are reversible. But the researchers also found that the switch between positive and negative effects on axon regrowth is directly related to the glial cells’ metabolic status.
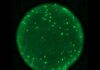
In follow-up experiments in flies, the researchers focused specifically on glycolysis—the metabolic pathway responsible for the breakdown of glucose—and discovered that upregulating this pathway alone in glial cells was sufficient to promote axon regeneration. “We show that glia can be reprogrammed to promote morphological and functional regeneration after CNS injury in Drosophila via increased glycolysis,” they wrote. This same result was observed in mice.
Further investigation in fly and mouse models led to the identification of two glucose metabolites, lactate and hydroxyglutarate, that act as key mediators of the glial switch from an inhibitory reaction to a stimulatory response. “Local application of L-lactate to injured spinal cord promoted corticospinal tract axon regeneration, leading to behavioral recovery in adult mice,” the scientists commented. Li further noted, “In the fly model, we observed axon regeneration and dramatic improvements in functional recovery when we applied lactate to damaged neuronal tissue. We also found that in injured mice, treatment with lactate significantly improved locomotor ability, restoring some walking capability, relative to untreated animals.”
Li and colleagues examined the specific pathway by which lactate and hydroxyglutarate act to enhance axon regeneration. Experiments revealed that when glial cells are activated, they release glucose metabolites, which subsequently attach GABAB receptors on the neuron surface and thereby activate pathways in neurons that stimulate axon growth. “Our findings revealed a metabolic switch to circumvent the inhibition of glia while amplifying their beneficial effects for treating CNS injuries,” the team concluded. “Our study demonstrated that administration of L-lactate locally to the lesion site of adult mammals promotes significant axon regeneration and functional recovery … L-lactate can influence axon regeneration by targeting GABAB receptor, which is widely expressed in neurons.”
Li further commented, “Our findings indicate that GABAB receptor activation induced by lactate can have a critical role in neuronal recovery after spinal cord injury. Moreover, this process is driven by a metabolic switch to aerobic glycolysis, which leads specifically to the production of lactate and other glucose metabolites.”
The researchers plan next to test the regenerative abilities of lactate and related molecules in larger animals and to determine which molecules are most effective for promoting regeneration. “The next phases of our work could set the stage for future translational studies in human patients affected by spinal cord injury,” Li added.