A gene therapy that modifies a patient’s own stem cells has shown promise against X-linked chronic granulomatous disease (X-CGD), the most common form of CGD, a hereditary immune disorder. Of the nine patients who received the gene therapy in a recent clinical trial, six are currently in remission and no longer receiving other treatments.
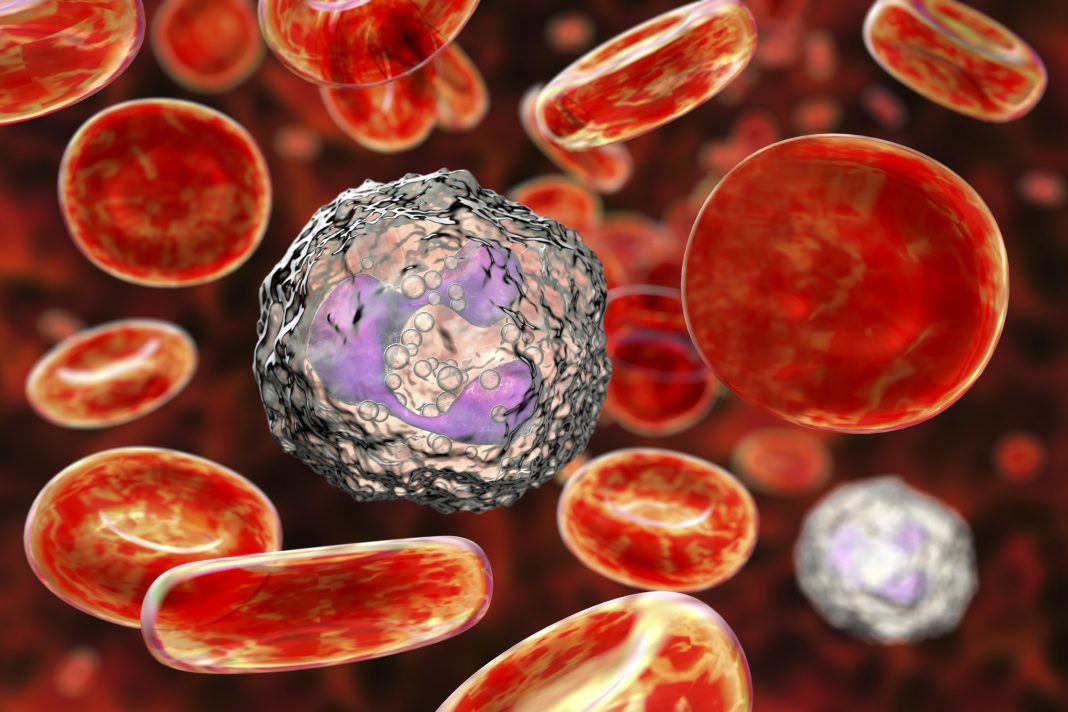
In this therapy, hematopoietic stem cells are removed from the patient’s bone marrow, genetically modified outside the body, and then reintroduced to the patient, where the modified cells mature into white blood cells that can produce the pathogen-killing compounds known as reactive oxygen species—immune-boosting chemicals that are lacking in untreated CGD patients. The therapy, if it proves to be effective in larger trials, would be an attractive alternative to an existing therapy that relies on bone marrow donations.
“With this gene therapy … cells are perfectly matched to the patient,” said Donald B. Kohn, MD, a stem cell researcher at the University of California, Los Angeles (UCLA). “It should be a much safer transplant, without the risks of rejection.”
Kohn is a co-corresponding author of a new article (“Lentiviral gene therapy for X-linked chronic granulomatous disease”) that describes the clinical trial. The article, which appeared January 27 in Nature Medicine, may remind readers of an earlier clinical trial, one that used a similar stem cell gene therapy to effectively cure a form of severe combined immune deficiency (also known as bubble baby disease) in more than 50 babies.
“The primary objectives were to assess the safety and evaluate the efficacy and stability of biochemical and functional reconstitution in the progeny of engrafted cells at 12 months,” the current article noted. “The secondary objectives included the evaluation of augmented immunity against bacterial and fungal infection, as well as assessment of hematopoietic stem cell transduction and engraftment.”
People with CGD have a genetic mutation in one of five genes that help white blood cells produce reactive oxygen species to destroy harmful bacteria and fungi that are ingested during phagocytosis. Without this defensive chemical burst, patients with the disease are much more susceptible to infections than most people. The infections can be severe to life-threatening, including infections of the skin or bone and abscesses in organs such as lungs, liver, or brain. X-CGD affects only males and is caused by a mutation in a gene found on the X-chromosome.
Other than treating infections as they occur and taking rotating courses of preventive antibiotics, the only treatment option for people with CGD is to receive a bone marrow transplant from a healthy matched donor.
“Patients can certainly get better with these bone marrow transplants, but it requires finding a matched donor,” Kohn explained. “Even with a match, there are risks.” Patients must take antirejection drugs for 6 to 12 months so that their bodies don’t attack the foreign bone marrow.
In the new approach, Kohn teamed up with collaborators at the United Kingdom’s National Health Service, France-based Genethon, the U.S. National Institute of Allergy and Infectious Diseases at the National Institutes of Health, and Boston Children’s Hospital. Another of the study’s co-corresponding authors, Adrian Thrasher, MBBS, PhD, professor, pediatric immunology and Wellcome Trust principal research fellow, led a team at Great Ormond Street Hospital (GOSH) to develop the viral delivery system for the X-CGD gene therapy.
The trial’s patients ranged in age from 2 to 27 years old. Four were treated at GOSH, and five were treated in the United States, including one patient at UCLA Health.
“Two enrolled patients died within three months of treatment from pre-existing comorbidities,” the Nature Medicine article detailed. “At 12 months, six of the seven surviving patients demonstrated stable vector copy numbers (0.4–1.8 copies per neutrophil) and the persistence of 16–46% oxidase-positive neutrophils. There was no molecular evidence of either clonal dysregulation or transgene silencing.”

An additional four patients have been treated since the new paper was written. All are currently free of new CGD-related infections and no complications have arisen.
Orchard Therapeutics, a biotechnology company of which Kohn is a scientific co-founder, acquired the rights to the X-CGD investigational gene therapy from Genethon. Orchard will work with regulators in the United States and Europe to carry out a larger clinical trial to further study this innovative treatment. The aim is to apply for regulatory approval to make the treatment commercially available, Kohn said.
Kohn and his colleagues plan to develop similar treatments for the other forms of CGD—caused by four other genetic mutations that affect the same immune function as X-CGD.
“Beyond CGD,” Kohn emphasized, “there are also other diseases caused by proteins missing in white blood cells that could be treated in similar ways.”