An international research team has identified a blood marker that they hope could form the basis of a cheap and simple test to predict and monitor the development of brain damage and neurodegenerative disorders such as Alzheimer’s disease, potentially a decade or more before symptoms manifest.
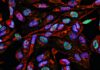
The protein, called neurofilament light chain (NfL) forms part of the internal skeleton of healthy brain cells, but is then found in the cerebrospinal fluid (CSF) and blood as a consequence of neuronal damage or death. Studies in families with an inherited, early-onset form of Alzheimer’s disease have now demonstrated how changing blood levels of NfL can predict the development and progression of brain damage and disease.
“It is not the absolute neurofilament concentration, but its temporal evolution, which is meaningful and allows predictions about the future progression of the disease,” said Mathias Jucker, PhD, a senior researcher at the German Center for Neurodegenerative Diseases (DZNE), and one of the lead researchers on the study, which is reported in Nature Medicine. “We were able to predict loss of brain mass and cognitive changes that actually occurred two years later.” In fact, differences in blood levels of the protein between individuals with a faulty version of the gene and relatives without the mutation were detectable 16 years before the affected participants were predicted to develop Alzheimer’s disease.
“Sixteen years before symptoms arise is really quite early in the disease process, but we were able to see differences even then,” added Washington University graduate student Stephanie Schultz, one of the paper’s co-first authors. “This could be a good preclinical biomarker to identify those who will go on to develop clinical symptoms.”
The researchers described their findings in a paper titled, “Serum neurofilament dynamic predicts neurodegeneration and clinical progression in presymptomatic Alzheimer’s disease.”
Changes to the brain can start many years before clinical symptoms of neurodegenerative diseases become apparent, the authors explained, but early detection is not routine. Alzheimer’s disease is characterized by cortical thinning and telltale toxic deposits of amyloid-β and tau. These pathological changes can be detected by magnetic resonance imaging (MRI), positron-emission tomography (PET), or by measuring levels of amyloid-β and tau protein in the CSF, but the latter requires an invasive spinal tap. “CSF collection is invasive and imaging modalities are expensive; therefore, they are not well suited to routine clinical practice,” the researchers stated. This means that diagnosis commonly is made only after symptoms develop.
While amyloid proteins are the focus of most developmental blood tests for Alzheimer’s disease, the DZNE and Washington University researchers have taken a different approach. “Our blood test does not look at the amyloid, but at what it does in the brain, namely neurodegeneration. In other words, we look at the death of neurons,” Jucker commented.
When brain cells die their remains can be detected in the blood. “Normally, however, such proteins are rapidly degraded in the blood and are therefore not very suitable as markers for a neurodegenerative disease,” Jucker added. “An exception, however, is a small piece of so-called neurofilament that is surprisingly resistant to this degradation.”
To investigate whether NfL levels in the blood could predict the progression of neurodegenerative disease the researchers turned to a cohort of families that participate in the Dominantly Inherited Alzheimer’s Network (DIAN), which is led by Washington University. Some of the family members carry rare genetic variants that cause Alzheimer’s disease to develop during the carrier’s 50s, 40s, or even 30s. A parent with a relevant mutation has a 50% likelihood of passing that mutation to their offspring, and any child who inherits the variant will almost inevitably develop symptoms of dementia at round about the same age as their parent. This gives researchers an opportunity to study what happens in the brain in the years before cognitive symptoms arise.
The researchers studied 405 people participating in the DIAN study, including 247 individuals who carried one of the early-onset genetic variants and 162 of their unaffected relatives. Each participant had previously undergone brain scans and cognitive tests. The scientists’ analyses showed that in individuals with a faulty gene, NfL levels were higher at baseline and also increased over time. In contrast, levels of NfL in unaffected relatives remained low and were largely steady. These differences in NfL levels were detectable 16 years before cognitive symptoms were expected to become evident in the mutation-carrying individuals. “Using serial NfL measurements we found that the NfL annual rate of change can distinguish non-carriers and mutation carriers as early as 16 years before the estimated symptom onset.,” the researchers wrote. “This is almost a decade earlier than when using absolute NfL levels measured at a single time point.”
The speed with which NfL levels rose also paralleled how the precuneus area of the brain, which is involved in memory, shrank and thinned. “In fact, precuneus thinning was also detected around 16 years before symptom onset, suggesting that NfL changes are sensitive enough to pick up such early regional brain atrophy,” the researchers stated.
They separately carried out a prospective evaluation of 39 patients to investigate whether blood NfL levels could predict cognitive decline. The results showed that individuals who exhibited a fast rise in blood NfL levels were more likely to show signs of brain atrophy and reduced cognitive abilities at a subsequent clinic visit two years later. “Although our prospective predication analysis was not adequately powered to demonstrate that NfL rate of change is indeed a better predictor of disease progression (neurodegeneration and cognitive decline) than absolute NfL values, our observations suggest that this is the case in presymptomatic Alzheimer’s disease, while absolute NfL levels are better predictors in the symptomatic phase,” the team stated.
Interestingly, while the rate of change of NfL concentration was closely associated with brain degradation, there was less correlation with amyloid protein deposition. This could indicate that neuronal degradation occurs independently to the amyloid deposition that triggers disease. “The association between NfL and cortical thinning, rather than amyloid-β deposition, is in line with cerebral amyloid-β aggregation being a trigger of subsequent neurodegeneration that, however, become independent of each other at later disease stages.”
“It will be important to confirm our findings in late-onset Alzheimer’s disease and to define the time period over which neurofilament changes have to be assessed for optimal clinical predictability,” said Jucker, who leads the DIAN study in Germany.
“This is something that would be easy to incorporate into a screening test in a neurology clinic,” said co-author Brian Gordon, PhD, an assistant professor of radiology at Washington University’s Mallinckrodt Institute of Radiology. “We validated it in people with Alzheimer’s disease because we know their brains undergo lots of neurodegeneration, but this marker isn’t specific for Alzheimer’s. High levels could be a sign of many different neurological diseases and injuries.” However, he acknowledged, “we’re not at the point we can tell people, ‘In five years you’ll have dementia.’ … We are all working towards that.”