![Group A Streptococcus bacteria (red) coat their surfaces with M1 proteins (white), which sequester and neutralize natural antibiotics produced by the human body. [UC San Diego Health]](https://genengnews.com/wp-content/uploads/2018/08/Oct15_2015_UCSanDiegoHealth_StrepSequestersAntimicrobial1118925420-1.jpg)
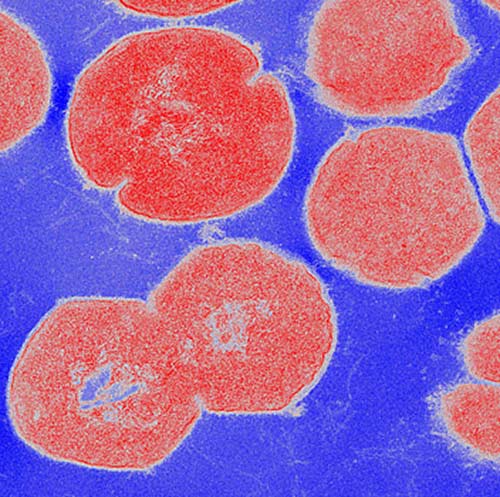
Group A Streptococcus bacteria (red) coat their surfaces with M1 proteins (white), which sequester and neutralize natural antibiotics produced by the human body. [UC San Diego Health]
The M1T1 strain of Streptococcus pyogenes is so virulent—and so notorious a cause of toxic shock-like syndrome and flesh-eating disease—that it has seized the attention of many scientists hoping to disarm it. These scientists have proposed various molecular mechanisms for M1T1’s depredations, but the pathogen still seemed to be hiding something up its sleeve, or sleeves.
The pathogen, as its name suggests, it is studded with M1 proteins, which reach out rather like tentacles. These tentacles, reports a group of scientists at the University of California, San Diego (UCSD), are not merely decorative, rather they account for the M1T1 strain’s exceptional ability to thwart a particular antimicrobial peptide, cathelicidin. This peptide, which is part of the innate immune system, is usually an effective pathogen killer, a piercer of microbial membranes and recruiter of infection-fighting cells. But it seems to treat M1T1 with kid gloves.
According to the UCSD scientists, M1 keeps cathelicidin at arm’s length. Its reach even extends to the cathelicidin precursor.
These results appeared October 14 in the journal Cell Host & Microbe, in an article entitled, “Group A Streptococcal M1 Protein Sequesters Cathelicidin to Evade Innate Immune Killing.”
“We show that the [Group A Streptococcus (GAS)] surface-associated M1 protein sequesters and neutralizes LL-37 antimicrobial activity through its N-terminal domain,” wrote the authors. “M1 protein also binds the cathelicidin precursor hCAP-18, preventing its proteolytic maturation into antimicrobial forms. Exogenous M1 protein rescues M1-deficient GAS from killing by neutrophils and within neutrophil extracellular traps and neutralizes LL-37 chemotactic properties.”
Essentially, Group A strep lacking M1 protein were easily killed by cathelicidin, but were rescued when they were armed with added M1 protein.
Following up on these results, the researchers evaluated cathelicidin in a mouse model of M1 strep skin infection. They found that it didn’t matter whether cathelicidin was present or not—the bacteria were just as virulent either way.
In contrast, M49, a less virulent strain of strep, caused larger skin lesions in mice lacking cathelicidin than in normal, cathelicidin-producing mice. This suggests that M49 is unable to hold off antimicrobial peptides the way M1 can, making the immune response more effective and the M49 bacteria less virulent.
“The famous strep M1 protein has been shown to have numerous virulence properties that aid in bacterial colonization, fool the immune system or provoke inflammation,” said the Cell Host & Microbe article’s senior author Victor Nizet, M.D., a UCSD professor of pediatrics and pharmacy. “We found that a major contribution of M1 protein to severe invasive infections can be explained by its ability to inactivate antimicrobial peptides.”
Other research groups previously reported that the M1 protein contributes to strep virulence because it makes it harder for immune cells to engulf the bacteria, or bind and inhibit other components of the immune system, such as antibodies. While those factors may apply to all Group A strep bacteria, it may be M1's ability to keep antimicrobial peptides at bay that makes strains with this version of M protein so deadly.
The findings underscore the need to fortify or optimize antimicrobial peptides in order to improve the immune system's odds of successfully fending off an infection, Nizet said. Understanding the interaction between M1 and antimicrobial peptides also provides a potential new approach to treating Group A strep infections.
“It's conceivable that we could find a drug that breaks the M1-antimicrobial peptide connection, unlocking the immune system's ability to fight the infection on its own,” said first author Christopher LaRock, Ph.D., a postdoctoral researcher in Dr. Nizet's lab.