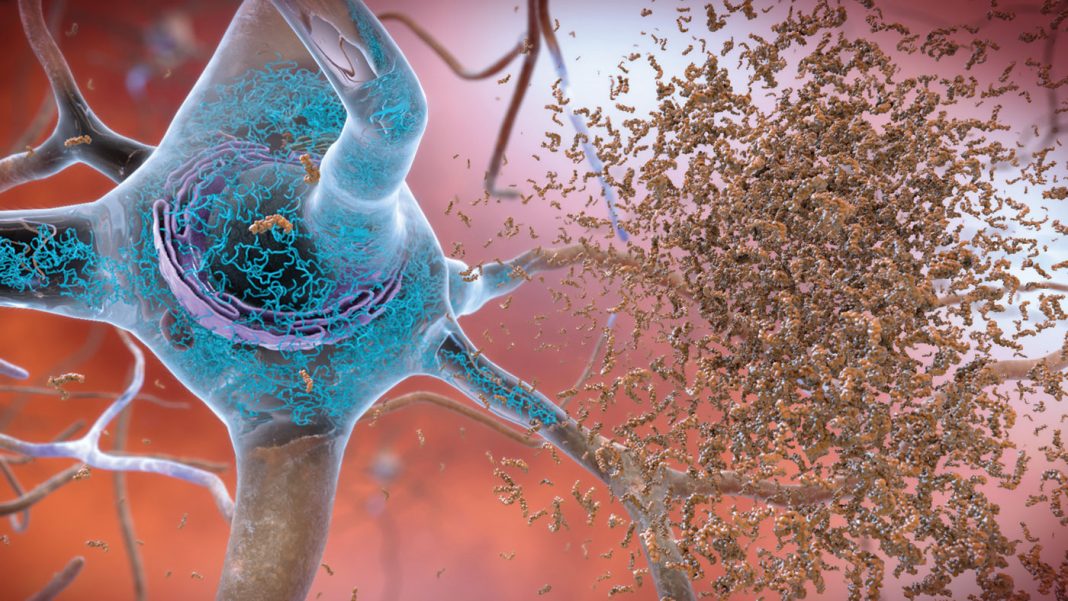
Neurons accumulate mutations more quickly in people with Alzheimer’s disease (AD) than in people without AD. Moreover, in AD, the mutations that accumulate in neurons, and that ultimately contribute to the death of neurons, show a distinctive pattern. Specifically, this pattern is consistent with elevated levels of reactive oxygen species (ROS), suggesting a link between the death of neurons and amyloid-β and tau—proteins that are known to accumulate in AD and induce the production of ROS.
These findings emerged from a study conducted by researchers at Boston Children’s Hospital, Brigham and Women’s Hospital, and the Broad Institute. After securing post-mortem frozen brain tissue samples from people with AD and from neurotypical people of similar age, the researchers isolated individual pyramidal neurons from the tissues and subjected them to single-cell whole genome sequencing. Ultimately, the researchers analyzed sequencing data from 319 neurons from the prefrontal cortex and hippocampus, areas that are important in cognitive functioning.
Detailed findings from this work appeared in Nature, in an article titled, “Somatic genomic changes in single Alzheimer’s disease neurons.” According to this article, normal neurons accumulate mutations primarily in an age-related pattern closely resembling the “clock-like” mutational signatures that have been previously described in healthy and cancerous cells. In neurons affected by AD, additional DNA alterations are driven by processes more like those seen with nucleotide oxidation, a process that is increased, the researchers observed, in AD-affected neurons in situ.
“Expressed genes exhibit signature-specific damage, and mutations show a transcriptional strand bias, which suggests that transcription-coupled nucleotide excision repair has a role in the generation of mutations,” the article’s authors wrote. “The alterations in AD affect coding exons and are predicted to create dysfunctional genetic knockout cells and proteostatic stress.”
So, people with AD not only have an abundance of newly acquired mutations in their neurons, but they also have enough to disable genes important to brain function.
“Cells have repair pathways to undo DNA damage, but our work shows that in AD, neurons can’t keep up with the repairs, so the damage is permanent and cumulative,” said Christopher Walsh, MD, PhD, chief of genetics and genomics at Boston Children’s Hospital and a co-senior investigator on the study. “This work provides a new way of thinking about neurodegenerative diseases such as AD, suggesting that they impair the ability of neurons to use their genome.”
Besides suggesting a role for nucleotide excision repair in the cascade of events that leads to AD, the study may also help connect the dots between the well-documented accumulation of amyloid-β and tau proteins in AD, and the loss of neurons.
The researchers not only found more mutations in AD-affected neurons, but differences between the pattern of mutations in AD-affected brains and the pattern of mutations in normally aging brains. These changes—switches in certain bases that make up DNA—were of a kind known to be induced by ROS, unlike mutations in normally aging brains. The team also found direct evidence of increased oxidation in the neurons of people with AD.
In addition to amyloid-β and tau, inflammation caused by microglia could also contribute to ROS production, noted August Yue Huang, PhD, an instructor at Boston Children’s Hospital and a co-first author on the Nature article. Microglia are immune cells in the brain that can interact with neurons, and have shown to be abnormally activated in AD.
“Neuroinflammation introduced by microglia might be one cause of oxidative damage to the genome,” Huang said.
The researchers indicated that genes important to brain function may be especially vulnerable to mutations. Essential genes used by the brain tend to be larger than average, presenting a bigger target that is more likely to be “hit” and disrupted. They are also more often turned on.
Genes with a higher level of expression in the brain are more likely to have critical functions. These very genes, Huang emphasized, “had a higher mutation burden.”
It’s tempting to speculate that antioxidants could have value in AD, but the researchers want to further investigate how oxidation of the genome occurs and the role that inflammation and immune reactions may play.
“We want to look at other neurodegenerative diseases like frontotemporal dementia, ALS, and chronic traumatic encephalopathy to see whether there’s a limit to the number of mutations in brain that a neuron can tolerate,” Walsh elaborated. “We’ve demonstrated that in AD, neurons cannot tolerate widespread oxidation of the genome, which results in permanent damage that can’t be fixed.”