Obesity risk factors of family background are associated with changes in the brain function, according to a study (“Obesity risk is associated with altered cerebral glucose metabolism and decreased μ-opioid and CB1 receptor availability”) published the International Journal of Obesity in conducted at the Finnish Turku PET Center.
The results show that the function of neural networks regulating satiety and appetite is altered already before a person develops obesity.
Obesity is linked to changes in brain insulin sensitivity and neurotransmitter function. These changes may explain increased appetite and overeating. However, thus far it has not been determined whether these changes are visible in the brain already before a person develops obesity, and if these changes would increase the risk for future obesity, says Tatu Kantonen, a doctoral student from the department of clinical medicine of the University of Turku.
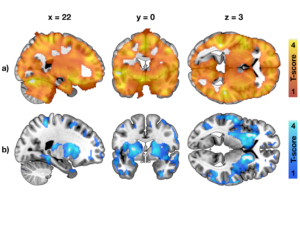
Kantonen’s study investigated changes in the brain in pre-obesity by studying the insulin, opioid, and cannabinoid function through PET imaging. The results showed that family-related risk factors such as parents’ obesity or diabetes were associated with altered insulin signaling in the subject’s brain as well as reduced function of the opioid and cannabinoid systems.
“In this triple-tracer positron emission tomography study, we investigated whether brain insulin signaling, μ-opioid receptors (MORs) and cannabinoid CB1 receptors (CB1Rs) are associated with risk for developing obesity.
“Subjects were 41 young non-obese males with variable obesity risk profiles. Obesity risk was assessed by subjects’ physical exercise habits, body mass index and familial risk factors, including parental obesity and T2D. Brain glucose uptake was quantified with [18F]FDG during hyperinsulinemic euglycemic clamp, MORs were quantified with [11C]carfentanil and CB1Rs with [18F]FMPEP-d2.
“Subjects with higher obesity risk had globally increased insulin-stimulated brain glucose uptake (19 high-risk subjects versus 19 low-risk subjects), and familial obesity risk factors were associated with increased brain glucose uptake (38 subjects) but decreased availability of MORs (41 subjects) and CB1Rs (36 subjects).
“These results suggest that the hereditary mechanisms promoting obesity may be partly mediated via insulin, opioid and endocannabinoid messaging systems in the brain.”
Disturbance in the neural networks controlling satiation and appetite can therefore be observed already before a person develops obesity, and these brain changes are connected to family-related risk factors of obesity. The results may have implications for the development of prevention and treatment interventions for obesity. They show that the brain and central nervous system are important targets in the treatment of obesity, explains Kantonen.







