Scientists at Genentech and the University of California have refined the sole mouse model of shigellosis to achieve a closer match to the hallmarks of the human disease. The development of this improved animal model is crucial for vaccine development efforts. At present, there is no vaccine against Shigella.
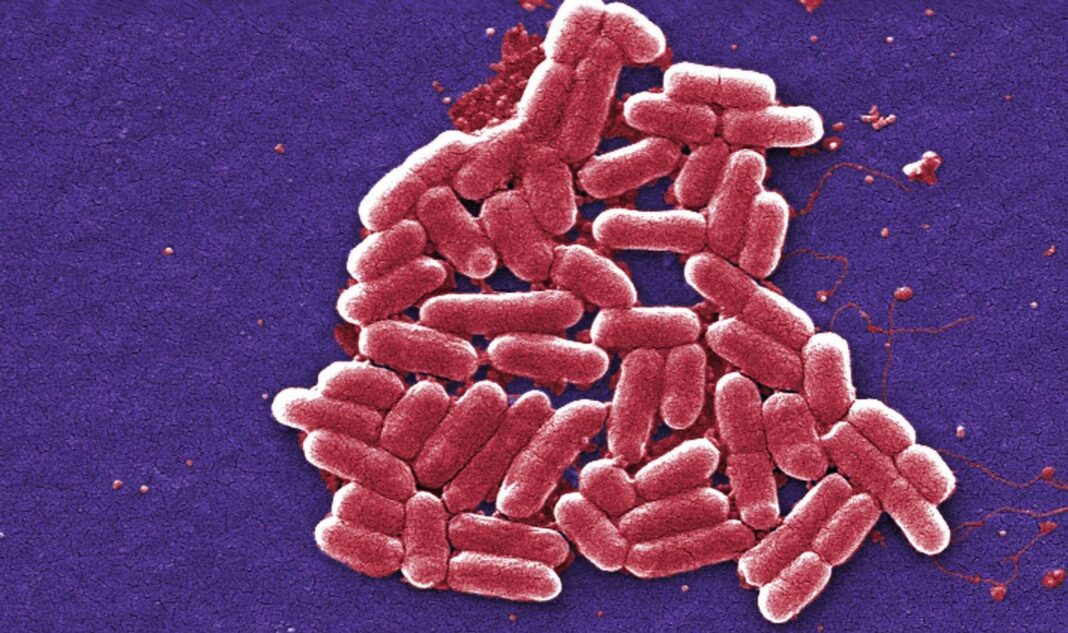
Shigella is a bacterium that infects intestinal cells causing hemorrhagic gastroenteritis (blood dysentery) in humans and other primates, but not in rodents.
The current study uncovers the mechanism underlying a Shigella virulence factor—an enzyme called IpaH7.8 that tags proteins with ubiquitin peptides to mark them for proteasomal degradation. The findings show IpaH7.8 inhibits a host pore-forming protein (GSDMD) that induces a form of programmed cell death called pyroptosis. Killing the infected cell eliminates the pathogen and its replicative niche, saving the host organism. Pathogens that evade this innate host defense mechanism stand a better chance of establishing infection.
The study shows IpaH7.8 can evade pyroptosis in humans but not in rodents, contributing to the species specificity of shigellosis. Shigella evades pyroptosis in humans since its IpaH7.8 can label GSDMD for degradation in humans but not mice. The authors showed that infecting human epithelial cells with Shigella lacking IpaH7.8 increases GSDMD mediated cell death.
Eliminating GSDMD in mice already primed for Shigella infection increased bacterial replication and disease severity, generating an improved model for human shigellosis.
These results are reported in the article, “Shigella ubiquitin ligase IpaH7.8 targets gasdermin D for degradation to prevent pyroptosis and enable infection,” published in the journal Cell Host & Microbe, this week.
“GSDMD-mediated pyroptosis is often part of the host’s primary defense mechanisms against microbial infections. This new work by the Dixit laboratory uncovers an interesting novel virulence mechanism that helps to explain how pathogenic Shigella strains cause shigellosis in humans,” said Mohamed Lamkanfi, PhD, professor of medical immunology at Ghent University, Belgium, and who was not involved in the current study.

Microbiome composition, innate immune signaling, and vulnerability to virulence factors determine a host’s susceptibility to Shigella infection. Giovanni Luchetti, PhD, lead author on the study and postdoctoral fellow in Vishva Dixit’s laboratory at Genentech, said, “Mice resist colonization of their gut upon oral administration of Shigella. This is overcome by pre-clearance of their commensal microorganisms with antibiotics. Still, mice resist infection by their detection of pathogen-associated molecular patterns (PAMPs) during Shigella invasion of the colonic epithelium.”
The authors showed critical determinants of innate immune signaling in the host, such as GSDMD, play a vital role in resisting Shigella virulence factors. “Whether mice have evolved these defense mechanisms as an environmental protective response to Shigella is unclear. In contrast, humans and non-human primates may simply represent a snapshot in evolutionary time where the arms race between pathogen and host currently favors Shigella,” said Luchetti.
Shigella evolved from Escherichia coli, a human commensal microorganism, which may partly explain why humans and other primates are its natural host reservoirs.
The research team also investigates why the enzyme IpaH7.8 can target the human but not the rodent GSDMD. “Subtle differences in GSDMD amino acid composition mapping to a solvent-exposed loop near the N-terminus are responsible for the selectivity of IpaH7.8 for human GSDMD. Surprisingly, these slight differences do not prevent a biochemical interaction of IpaH7.8 and either mouse or human GSDMD. However, this region does appear to influence the subsequent ubiquitination reaction that is catalyzed by IpaH7.8 to allow modification of only human GSDMD,” said Luchetti.
Can preventing IpaH7.8 mediated human GSDMD degradation, act as a prophylactic against Shigella infection in humans? “Whether targeting IpaH7.8 constitutes a viable therapeutic strategy in humans awaits further examination. However, given the protection that GSDMD affords mice, development of IpaH7.8 inhibitors may indeed represent an important therapeutic opportunity worth pursuing,” said Luchetti.
“The discovery that Shigella exploits the host’s proteasome machinery to its own advantage and degrades GSDMD to prevent pyroptosis of infected cells appears conceptually reminiscent of the emerging PROTAC (proteolysis targeting chimera) therapies that aim to target disease-causing proteins for proteasomal degradation,” added Lamkanfi. “Given this parallel, it’s tempting to speculate that these novel insights from the Dixit laboratory may inspire the development of GSDMD-degrading PROTAC agents as a therapeutic strategy to inhibit pyroptosis in inflammatory diseases in which GSDMD activity may contribute to disease pathologies, such as in Familial Mediterranean Fever (FMF) and Cryopyrin-associated periodic syndromes (CAPS).”
Shigella is not the only pathogen that has devised a ploy to defy death-inducing mechanisms of the infected host cell by targeting GSDMD. “To date, three such examples have been reported including our own study on Shigella IpaH7.8, and two viral GSDMD inhibitors encoded by Enterovirus 71 and SARS-CoV-2. Modulation of host immune signaling by pathogen-mediated ubiquitination appears to be a widespread virulence strategy,” Luchetti said.
Luchetti added that their work has benefited tremendously from the sole mouse model of shigellosis recently developed by Russell Vance’s lab at the University of California at Berkeley. Earlier, mice models of shigellosis were generated by inoculating through the nasal cavity or the peritoneal sac instead of the natural route of oral ingestion.
As a next step to the study, the team will explore additional factors encoded by Shigella that help the pathogen establish infection in humans. To better understand the selectivity of IpaH7.8 for human GSDMD, the team intends to pursue structures of the complexes that form between IpaH7.8 and human and mouse GSDMD.
“From a population genetics standpoint, given how only subtle differences between human and mouse GSDMD determine IpaH7.8 sensitivity, it will be worthwhile to investigate whether IpaH7.8-resistant variants of GSDMD have emerged,” said Luchetti. “With the most accurate model of human disease in hand, greater efforts should be made to develop a sorely needed Shigella vaccine.”