May 15, 2013 (Vol. 33, No. 10)
Caitlin Smith
The process of discovering new drugs is mainly linear—and prone to bottlenecks. Putting a new drug on the pharmacy shelf may take well over a decade, which spells a waste of time and money if the drug fails once it reaches the market.
Drug repositioning (or repurposing), however, promises to be faster and cheaper. In drug repositioning, researchers search already-approved drugs to see if they might have a hitherto unforeseen effectiveness against particular diseases (unrelated to the conditions against which they were originally developed).
Because the approved drugs have already been tested in humans, repositioning a drug saves time. Important information such as toxicity, pharmacology, and dosage details, for example, have already been gathered. Many repositioned drugs can move straight into Phase II trials, and can thus meet the needs of patients sooner, and with lower costs.
Drug repositioning can result in researchers learning more about a drug’s mechanisms of action, or the biology of the pathway it affects—and sometimes leads to new and more promising drug compounds. Today, scientists are pursuing various types of drug repositioning.
Computational biology is key to the repositioning methods used by Yves Lussier, M.D., professor of medicine and engineering, and director of the Institute for Interventional Health Informatics at the University of Illinois at Chicago. Dr. Lussier and colleagues use “hypothesis-anchored computational biology” to study drug repositioning, which begins with making hypotheses about how a repositioning might work.
“We use network-based repositioning to find aberrant re-entry mechanisms, which is conceptually different from pathway-based,” he says. For example, for interacting proteins, they would examine the literature for known published interactions, knowledge bases such as KEGG (Kyoto Encyclopedia of Genes and Genomes) and GO (Gene Ontology project), and results from yeast-2-hybrid studies. Alternatively, they may use genome-wide repositioning with GSEA (Gene Set Enrichment Analysis).
Dr. Lussier suggests that there is room to grow in this field of research. Despite the available funding, he says that a limited number of researchers have the experience and skills required not only to apply computational biology to drug repositioning, but also to interpret the biological context and see the drugs through clinical trials. “The biggest challenge is to empower the right groups and establish the most cost-efficient approaches to reposition drugs,” he says.
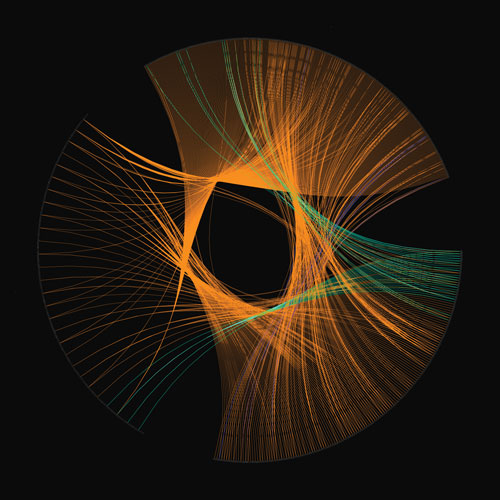
University of Chicago scientists have uncovered the basic principles of cross-talk between pathways. This image was produced from reverse engineering significant molecular pathways associated to protein domains and molecular functions of their constituent molecules. A few pathways and their associations are shown in orange. Each point on the circle corresponds to a distinct entity.
Researchers at Biovista are also using impressive computational power for drug repositioning. Their Clinical Outcome Search Space™ (COSS) technology ranks how relevant clinical outcomes (more than 29,000 of them) might be against all drugs, and against all human molecular targets. It can also analyze the relevance of all drugs against diseases of interest.
“COSS combines experimentally derived data about on- and off-target pharmacology with data from multiple sources about every drug, every indication, and every adverse effect, to generate unique data profiles for every drug, disease, adverse event, or human molecular target,” says Biovista’s president, Aris Persidis, Ph.D. “COSS then compares and ranks the data profiles to determine the most relevant ones, which are then validated experimentally.”
Biovista has already repositioned two drugs for the progressive form of multiple sclerosis (MS), which has had few treatment options. Most MS drugs, for treatment of the relapsing-remitting form of MS, compromise the patients’ immune systems and have significant side effects. Biovista wanted to find non-immunomodulatory drugs that would treat the neurodegeneration that occurs in the progressive form of MS.
COSS found an unknown role of mitochondrial dysfunction in MS, which previously had been thought a purely autoimmune disease. Therefore they used COSS to reposition drugs against mitochondrial—rather than autoimmune—dysfunction, resulting in two drug candidates (BVA-101 and BVA-201) that they then validated as effective in animal models of MS.
“COSS was thus able to help redefine the potential mechanism of the disease, opening up fresh new opportunities for unanticipated therapies,” says Dr. Persidis. “Biovista is currently designing first-in-human studies for its MS program candidates.”

Using existing drugs in new ways to probe biological function can increase our ability to understand disease. [Biovista]
Understanding Mechanisms
Indeed, not only are mechanisms important for drug repositioning, but we can also gain new insights into previously unknown mechanisms in the process. “In my opinion, mechanistic understanding is essential for the success of drug repositioning,” says Stephen Wong, Ph.D., chairman for department of systems medicine and bioengineering at the Methodist Hospital Research Institute, and director of the NCI Center for Modeling Cancer Development.
Dr. Wong’s group uses an integrative approach that combines bioinformatics analysis, pathway reconstruction, high-throughput and high-content screening, and chemi-informatics methods to look at drug targets and pathways of the disease of interest. They follow this by validating the drugs in in vitro and preclinical experiments.
“Many drug repositioning methods still follow a conventional hypothesis-driven approach, testing one drug or one target pathway at a time,” says Dr. Wong. “This does not take advantage of large amounts of data on many diseases and drugs available on the web and various public databases, nor the high-throughput biological automation capability today.”
A characteristic of Dr. Wong’s research is his emphasis on mechanistic understanding, which he says is lacking in research that uses a more data-driven approach.
“Many of those studies do not provide mechanism reasoning, nor uncover new potential targets not found in existing commercial or public databases,” he says. In contrast, his approach relies on a mechanistic interpretation, including molecular pathways or gene regulatory networks, as to a particular drug’s newfound effectiveness against a particular disease.
“We developed a unique, network motif-based method to extend generic pathways in existing databases or literature into pathways of specific subtype of diseases of interest,” he says. “We also developed an integrative web-accessible database, DrugMap Central, to support efficient online querying and visualization of multidimensional drug information for repositioning studies, and identifying the application of known drugs and compounds to new indications or diseases.”
Dr. Wong’s group recently worked with oncologists to reposition two drugs for new roles against cancer: sunitinib (previously used for imatinib-resistant GIST and renal cell carcinoma) for breast cancer brain metastasis, and chloroquine (previously used for malaria) for triple-negative brain metastases, now in Phase II trials.
Balancing Act
Weighing the benefits of a drug against its undesirable side effects can make for an intricate balancing act, practiced daily by Mike Pollastri, Ph.D., associate professor in chemistry and chemical biology at Northeastern University. Dr. Pollastri’s group works on repositioning drugs for neglected tropical diseases such as sleeping sickness. They compare the parasite genome to the human genome, and look for targets and pathways that parasites and humans have in common.
“Then we look for human drugs that target the closest homologous parasite molecules,” says Dr. Pollastri. “So if there’s a certain enzyme in a parasite, and we know that there is a drug that targets a homologous enzyme in humans, we would go after that one first.” Next they test those drugs against the parasites, and then use the drugs as a starting point for drug discovery.
Dr. Pollastri calls it target class repurposing, in which a human drug that acts on a homologous parasitic target is used to begin developing an even more effective drug specifically against the parasite. They usually re-optimize the drug for enhanced functioning in the parasite, such as tweaking the dosage or solubility. “For sleeping sickness, often we have to re-engineer drugs so that they get into the brain,” says Dr. Pollastri. “We use the drugs themselves as a starting point, but we don’t repurpose the drugs themselves.”
Recently they discovered that a drug made by Novartis, currently in clinical trials for cancer, is also extremely potent against sleeping sickness. Another repositioned drug, commonly used in Africa for sleeping sickness, was a failed cancer drug from the 1980s. Both cancer drugs target the same class of enzymes, decarboxylase inhibitors, that function both in mammalian cells and in parasites.
One of the important optimizations they must wrestle with is the delicate balance between effectiveness, and the tolerance level for patient side effects. For example, PDE4 inhibitors kill parasites, but they also cause nausea and vomiting in humans, so this must be balanced with efficacy.
“The biggest challenge is always going to be finding compounds that are effective against a parasitic infection and balancing that with the side-effect profile and the primary effect profile in humans,” says Dr. Pollastri. Another example is one of the main drugs used against sleeping sickness, melarsoprol. “Melarsoprol kills 5% of the patients,” he says. “It’s an arsenic compound. But the disease itself will certainly kill you if you’re not treated.”
Regardless of the method, an important step of the repositioning process is validation. “We are particularly happy to enjoy the benefit of validation by collaboration,” says Dr. Persidis, referring to Biovista’s partnerships with both pharmaceutical companies and patient advocacy groups representing different diseases.
“This exposure, together with our internal programs, is helping us stay at the forefront of repositioning research, both in terms of the COSS technology itself, and also in terms of advancing individual programs in our areas of interest,” he says. Indeed, Dr. Wong says that one thing above all else is key: “Validation, validation, and validation—or else all big data or systems biology approaches are academic exercises.”







