By Jinping Lai, PhD, and Jing Shi, PhD
Chimeric antigen receptor (CAR) T-cell therapies hold great promise for the treatment of both hematologic cancers and solid cancers. However, they also pose unique challenges for bioanalysis. For example, different CAR T-cell therapies designed to treat different cancers typically require different testing regimes. Another challenge is that regulatory expectations for CAR T-cell therapies are in flux.
When faced with daunting bioanalysis challenges, developers and sponsors of CAR T-cell therapies needn’t “go it alone.” They can keep their programs on track by partnering with companies that offer specialized laboratory services. Partner candidates should be able to help clients navigate the issues summarized in this article.
CAR T-cell therapy basics
In CAR T-cell therapies, the T cells are infected ex vivo with replication-deficient retro- or lentiviruses that carry a gene for an engineered receptor. Once injected into patients, the modified T cells recognize, attack, and kill cancer cells. Also, the modified T cells continue to replicate.
CAR T-cell therapies can be autologous or allogeneic. The latter raises the risk of graft-versus-host disease. To reduce this risk, developers are exploring possibilities such as the use of gene editing technologies for producing CAR T cells that lack certain native T-cell receptors on their surface.
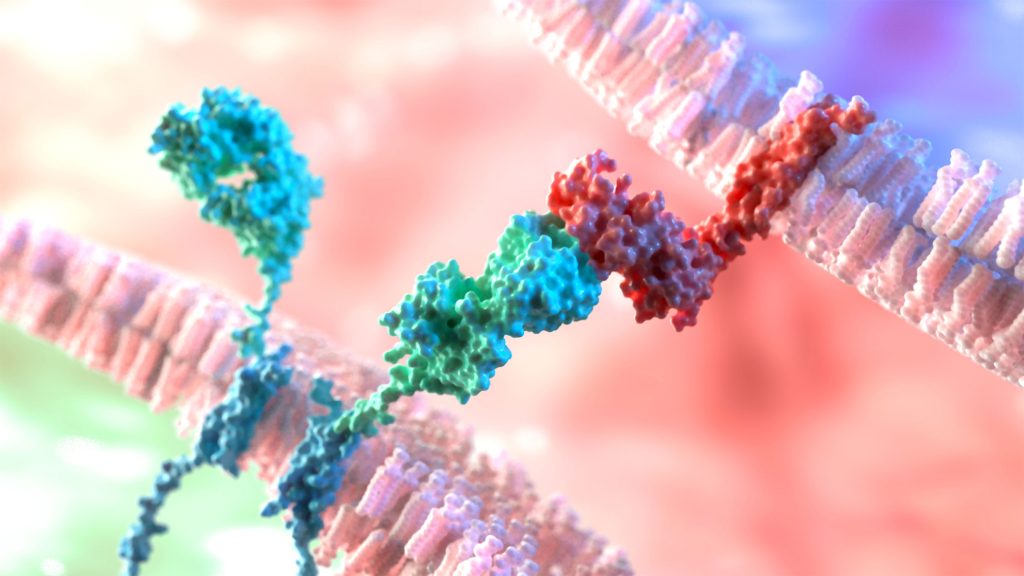
CARs have an antigen-binding ectodomain, a transmembrane domain, and an endodomain. (The ectodomain may incorporate a single-chain variable fragment, or ScFv, a kind of engineered antibody fragment that can recognize cancer cell membrane proteins.) To date, five generations of CARs have been introduced. Each new generation is meant to outperform the previous generation in terms of persistence, proliferation, safety, and efficacy.1
Key bioanalysis components
To assess the quality of CAR T-cell therapies and satisfy regulatory requirements, researchers test for immunogenicity and pharmacokinetic (PK) characteristics. For CAR T-cell therapies that progress to late-stage clinical trials, it is also necessary to identify biomarkers that can predict patient outcomes and optimize product characteristics.
Bioanalysis typically includes the following tasks:
- Immunogenicity assays to analyze a CAR T cell’s likelihood of provoking an immune response.
- PK assays to determine how CAR T cells move throughout the body and are cleared.
- Tests for replication competent lentivirus to address recombination risks. (These tests should be performed during CAR T-cell manufacturing or prior to administration.)
- Gene copy number analyses to limit toxicity. (The dynamic range should cover five or six orders of magnitude.2)
Bioanalysis methods
CAR T cells pose unique considerations for bioanalysis. Consequently, traditional bioanalysis methods often fall short. The traditional method known as the ligand-binding assay (LBA) measures the interaction between two molecules (antigen and antibody) to quantify therapeutics, assess biomarkers, and detect anti-drug antibodies (ADAs). To date, many LBA-based CAR T-cell ADA assays have been developed on the ScFv. However, due to the artificial nature of the LBA setup and the inability to fully represent the extracellular domain of the CAR, the LBA may lack sensitivity to immunogenicity risk factors or miss them altogether.
In CAR T-cell bioanalysis, flow cytometry is preferred for both PK testing and ADA detection because the method is fast, accurate, and highly efficient. Patients should be monitored longitudinally to determine whether and to what extent their CAR T cells replicate. So far, the target antigens for the FDA-approved CAR T-cell therapies are B-cell based, such as a CD-19 or BCMA.
Key questions to ask a laboratory testing partner include:
- What bioanalytical testing methods are available?
- Which methods best support the gene of interest?
- What kinds of support can the laboratory testing partner offer through the submission phase?
- What advanced bioanalytical techniques are available to analyze critical parameters?
Cytokine analysis is also very important in bioanalytical evaluations because it determines the potential for cytokine release syndrome. Cytokine profiling can be performed with traditional assays such as ELISA, MSD, Luminex, and SIMOA. For more thorough profiling, a combination of assay platforms can be used.
Method development must be standardized during discovery for each gene of interest. Researchers must have the primer, that is, a short strand of RNA or DNA, to conduct qPCR testing and standardize assay conditions. Transfection efficacy must also be examined.
Timelines and regulatory considerations
The time needed to develop and validate bioanalytical methods for CAR T cells typically exceeds that for ligand-binding assays. The cell surface of CAR T cells requires comprehensive understanding of the CAR’s structure, solubility, and binding nature. LBA approaches (based on soluble CAR or complete extracellular CAR) as well as cell-based and flow cytometry approaches are available for ADA assays. Flow cytometry and qPCR are the most effective platforms for PK assessment.
It usually takes between two and six months and multiple types of assays to overcome multiple challenges such as endogenous receptor/ligand interactions that interfere with CAR binding. To assess the sensitivity and reproducibility of CAR transgenes in CAR T cells, ddPCR can be used to minimize the sample matrix effect, increase rare event detection, and reduce variation over time. The longer the duration of bioanalysis, the greater the need to budget it into program timelines.
Regulatory guidance for CAR T-cell therapy is still evolving. Nonetheless, documents such as the white paper released in 2021 by the Workshop on Recent Issues in Bioanalysis help inform research methodologies and add breadth to the regulatory knowledge base.3 In the white paper, researchers outline recommendations for several topics, including endogenous compounds, complex specifications, regulated mass spectrometry, and biomarkers.
With CAR T-cell therapies, as with many novel drugs, initial submissions establish the baseline for testing methodologies and define the pathways for subsequent regulatory approval. There are currently more robust guidelines for treatments aimed at blood cancers than for treatments aimed at solid tumors; the guidelines that have been published exist in part because of predicate drugs.
For example, before Novartis gained approval for its B-cell acute lymphoblastic leukemia treatment tisagenlecleucel in 2017, it endured a very lengthy regulatory process. But when Gilead gained approval for brexucabtagene autoleucel to treat relapsed or refractory mantle cell lymphoma just three years later, the regulatory process was greatly accelerated because regulators had already provided initial guidance. FDA regulators also routinely initiate collaborations with drug developers to create mutually beneficial guidance documents.
To date, the FDA has approved six CAR T-cell therapies—ciltacabtagene autoleucel, idecabtagene vicleucel, lisocabtagene maraleucel, tisagenlecleucel, brexucabtagene autoleucel, and axicabtagene ciloleucel. The FDA issued considerations for developing CAR-T cell products in March 2022, which gives drug developers and sponsors specific guidance around CMC pharmacology and toxicology and clinical study design.4 With every new submission, the regulatory pathway becomes more defined, providing regulators with more data and business cases to draw upon.
Future cell-based therapies
Modified stem cells can serve as drug delivery vehicles. (For example, neural stem cells can be engineered to deliver anticancer agents to brain tumors.) Also, stem cells can be altered into other types of cells, including B cells, T cells, or NK cells.
Methods to create NK cells from stem cells are particularly promising even though they are time consuming. The times required at present are tolerated because NK cells from patients cannot be harvested in sufficient numbers.
Allogenic treatments are also evolving. By modifying T cells from healthy donors, researchers sidestep issues of functional fitness of a patient’s T cells. Allogenic CAR T-cell therapies also allow for multiple modifications and CAR combinations to target multiple tumor antigens.
A final word
CAR T-cell therapies represent an emerging field in medicine, one that must deal with evolving regulations and distinct bioanalytical requirements. Because CAR T cells present immunogenicity risks that traditional methods such as LBAs may fail to recognize with adequate sensitivity (or miss altogether), diverse and innovative methods are required. An experienced laboratory partner can offer novel assays and expert guidance to help drug developers and sponsors navigate the process.
References
- Funfrock P. From the first to the fifth generation of CAR-T cells. ProteoGenix. Published August 3, 2021. Accessed October 7, 2022.
- Shi J, Chen X, Diao J, et al. Bioanalysis in the Age of New Drug Modalities. Am. Assoc. Pharma. Sci. J. 2021; 23(3): 64. DOI: 10.1208/s12248-021-00594-w.
- Kaur S, Alley SC, Szapacs M, et al. 2021 White Paper on Recent Issues in Bioanalysis. Bioanalysis 2022; 14(9): 505–580. DOI: 10.4155/bio-2022-0078.
- U.S. Food and Drug Administration. Considerations for the Development of Chimeric Antigen Receptor (CAR) T Cell Products: Draft Guidance for Industry. Published March 2022. Accessed August 2022.
Jinping Lai, PhD, is director of large molecule bioanalysis and Jing Shi, PhD, is vice president and global head of bioanalytical services at WuXi AppTec.





