Researchers at the University of Queensland in Australia have identified a small molecule that can stop the progression of Parkinson’s disease (PD) and improve motor function in multiple mouse models. The team says human trials with an optimized compound could start within the next couple of years.
The prototype molecule, MCC950, blocks an immune system target, the NLRP3 inflammasome, which the researchers’ investigations showed is activated in the brains of PD patients and animal models. These studies, reported in Science Translational Medicine, indicated that chronic NLRP3 activation may be a key mechanism that drives the pathology of PD and dopaminergic neurodegeneration.
“We found a key immune system target, called the NLRP3 inflammasome, lights up in Parkinson’s patients, with signals found in the brain and even in the blood,” says research lead Trent Woodruff, Ph.D., an associate professor at the University of Queensland faculty of medicine. Referring to studies in mice he adds, “MCC950, given orally once a day, blocked NLRP3 activation in the brain and prevented the loss of brain cells, resulting in markedly improved motor function.”
Describing their results in a paper titled, “Inflammasome inhibition prevents α-synuclein pathology and dopaminergic neurodegeneration in mice,” the team suggests that inhibiting NLRP3 may present “a promising therapeutic strategy to mitigate progressive dopaminergic degeneration in PD.”
PD is the second most common neurodegenerative order worldwide, and affects about 2% of the population aged over 60 years, the authors write. The disease is characterized by loss of dopaminergic neurons in the substantia nigra area of the brain, together with chronic neuroinflammation, mitochondrial dysfunction, and accumulation of misfolded α-synuclein-rich protein aggregates that form characteristic Lewy bodies. While current treatments can help to manage symptoms, they don’t address the disease process itself. “Current therapies for PD, including levodopa treatment and deep brain stimulation, can manage symptoms but have little to no impact on the underlying disease pathology,” the authors state. “Therefore there is an urgent need to develop therapeutic strategies that halt or impede disease progression.”
Chronic microglial neuroinflammation is found in the brains of living patients with early PD, as well as in post-mortem brains. “Compelling evidence from clinical, preclinical, and epidemiological studies supports a pathogenic role for chronic neuroinflammation during dopaminergic degeneration,” the team states. What hasn’t yet been discovered is a mechanism linking α-synuclein pathology, progressive dopaminergic neuronal death, and chronic microglial neuroinflammation.
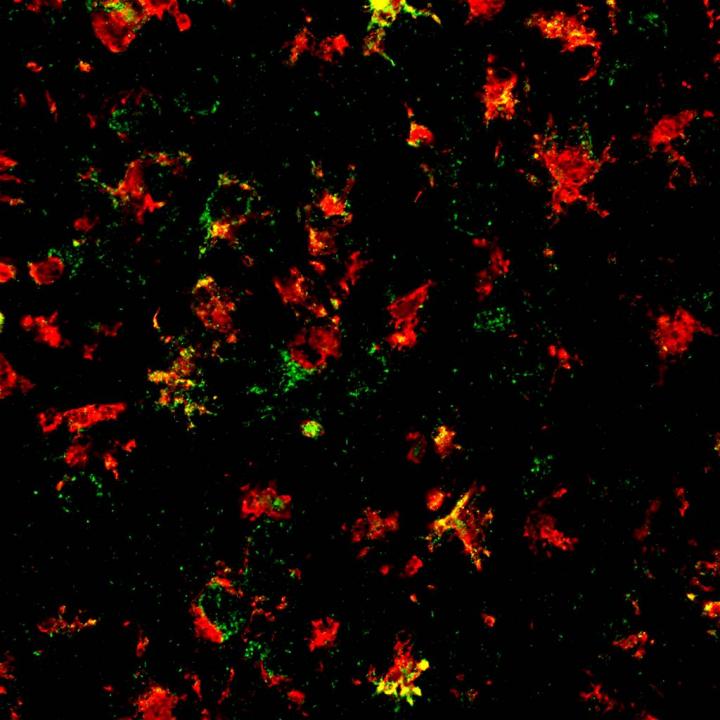
Inflammasomes, including NLRP3, are multiprotein complexes that act to sense and monitor environmental and cellular stress. Dr. Woodruff’s team claims that their new studies provide direct evidence for NLRP3 inflammasome activation in the post-mortem brains of PD patients and in multiple rodent models, characterized by fibrillar α-synuclein pathology. The results point to reactive microglia as the source of NLRP3 inflammasomes in human PD patients.
Their initial investigations confirmed NLP3 upregulation in the postmortem brains of PD patients, and increased inflammasome activation at the sites of dopaminergic cell loss. “Our results provide compelling clinical evidence for inflammasome activation in postmortem PD brains, confirming that key inflammasome markers are elevated in the substantia nigra of patients with PD,” they note. NLRP3 inflammasome activation was also identified in different animal models of PD that are characterized by dopaminergic degeneration driven by mitochondrial dysfunction, oxidative stress, or α-synuclein pathology.
Further studies in these mouse models indicated that fibrillar α-synuclein effectively triggers IL-1β secretion by microglia and NLRP3 activation. “ … fibrillar α-synuclein mediates a delayed but robust activation of the inflammasome pathway in microglia,” the team writes. In contrast, α-synuclein did not stimulate the release of IL-1β from microglia obtained from NLRP3-knockout mice.
Studies in a mouse model known as PFF that recapitulates many of the key features of Lewy body pathology in PD showed that NLRP3 inflammasome activation occurs at an early stage of neuropathology, which the authors say indicates that chronic microglial NLRP3-driven mechanisms play a “crucial role” in the propagation fibrillar α-synuclein pathology.
Having demonstrated NLRP3 activation in human PD brains and in animal models, the team then tested the effects of blocking NLRP3 activation using a small molecule inhibitor, MCC950. This approach differs from more traditional attempts to develop new treatments for Parkinson’s disease, which have focused on blocking the build-up of toxic proteins. “… we have taken an alternative approach by focusing on immune cells in the brain called microglia that can clear these toxic proteins,” comments co-author Matt Cooper, Ph.D., professor at the University of Queensland Institute for Molecular Bioscience. “With diseases of aging such as Parkinson’s, our immune system can become over-activated, with microglia causing inflammation and damage to the brain.”
MCC950 (originally referred to as CP-465773) is one of a class of sulfonylurea-containing compounds that were initially reported as inhibitors of IL-1β post-translational processing, the authors explain. Their in vitro tests confirmed that MCC950 blocked mediators of microglial inflammasome activation by α-synuclein aggregates. Encouragingly, tests in multiple animal models of PD also showed that oral administration of nanomolar amounts of MCC950 resulted in improved motor function, and protected animals against the loss of dopaminergic neurons.
“Oral MCC950 treatment effectively blocked NLRP3 activation in all PD models that we tested, irrespective of the distinct upstream triggers in these models,” the researchers comment. “MCC950 effectively ‘cooled the brains on fire’, turning down microglial inflammatory activity, and allowing neurons to function normally,” Dr. Cooper states.
Further analysis of mouse brain tissue confirmed that MCC950 was associated with reduced α-synuclein aggregation “… pharmacological inhibition of NLRP3 with an orally active, CNS-permeable inhibitor can protect against dopaminergic degeneration in vivo in rodent models of PD, confirming a pathologic role for NLRP3 inflammasome activation in driving disease progression in mice,” the authors conclude. “Our results demonstrate that the NLRP3 inflammasome plays a key role in PD-like pathophysiology in rodents and might represent a feasible therapeutic target to mitigate neurotoxic α-synuclein pathology and the resulting nigrostriatal dopaminergic neuron loss in PD.”
They state that while lapsed patent issues mean that MCC950 won’t itself represent a commercially viable therapeutic candidate for treating PD, improved follow-on compounds have been developed that could be taken into the clinic for treating neurodegenerative diseases. “We have used this discovery to develop improved drug candidates and hope to carry out human clinical trials in 2020,” Dr. Woodruff notes. And as the authors conclude, “the potency and specificity of MCC950 for NLRP3 inhibition in the CNS, combined with its neuroprotective efficacy and safety profile after long-term oral dosing, make it an excellent lead for optimization of drug candidates and potential clinical translation in PD.”