Samples from over 1,800 patients showed high level of key transcription factor in cancer cells was associated with reduced survival.
Measuring levels of the multifaceted transcription factor heat-shock factor 1 (HSF1) or its mRNA in breast cancer samples represents an accurate, independent prognostic indicator of poor outcome, scientists claim. Tests on tumor tissue and adjacent healthy tissue from nearly 2,000 breast cancer patients indicated that HSF1 accumulates in the nucleus in cancer cells, and its presence and level were associated with increased mortality.
The Whitehead Institute for Biomedical Research-led team found the relationship was independent to other variables, and was particularly strong for ER-positive cancers. Their work is described in PNAS in a paper titled “High levels of nuclear heat-shock factor 1 (HSF1) are associated with poor prognosis in breast cancer.”
The transcriptional regulator HSF1 is a master controller of the cellular response to a wide variety of stressors, driving the production of classic heat shock proteins (HSPs) that act as protein chaperones, but also controlling the expression of numerous other genes involved in cell survival under stress conditions, the researchers explain.
The Whitehead-led team’s previous work has shown that HSF1 is in addition co-opted by cancer cells to help them cope with malignancy-associated changes in cellular physiology and the tumor microenvironment, resulting in what they term “enhanced proliferation and increased fitness of malignant cells as they emerge.”
HSF1 normally shuttles between the nucleus and the cytoplasm, but on activation by stressors increasingly accumulates within the nucleus. Research by Susan Lindquist, Ph.D.’s team on human breast cancer samples had previously observed a striking shift in the localization of HSF1 from the cytoplasm to the nucleus, and their work in mouse models led to the hypothesis that an increase in nuclear HSF1 might be a marker of poor prognosis.
To investigate this notion further, the team has now examined the relationship between HSF1, clinicopathological characteristics, and survival outcomes in 1,841 breast cancer patients enrolled in the Nurses’ Health Study.
They first tested the specificity of a commercially available HSF1 antibody cocktail on samples from hsf1 wild-type and null mice, and then examined the expression of HSF1 in invasive carcinoma and matched normal adjacent breast tissue from seven patients, using immunoblot analysis. In every case the more HSF1 in the tumor samples than in the matched control samples.
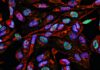
HSF1 is only active in the nucleus, so the researchers next used IHC to look at the localization and expression levels of HSF1 in a few dozen tumor cells and matched normal cells. The results highlighted a major difference between malignant cells and the adjacent normal breast tissue, in that none of the normal tissue demonstrated any nuclear HSF2, whereas there was nuclear staining in the majority of breast tissue samples. “The increase in HSF1 levels in invasive tomors supported the concept that HSF1 is activated in the malignant state,” they remark.
Moreover, the intensity of HSF1 expression was uniform among the tumors, independently to factors such as the position of the tumor cells in the cancer, or distance from vasculature. This uniformity contrasts with the variable patterns seen with most prognostic markers evaluated in human tumor sections using IHC, and indicates that the increase in HSF1 in tumor cells is primarily due to internal, cell-autonomous factors rather than external microenvironmental stress, they add.
Dr. Lindquist et al. then evaluated 1,841 invasive breast cancer cases from the NHS from HSF1 localization and expression. Cases were scored by a semiquantiative assessment of nuclear staining intensity. Four hundred and four cases were negative for nuclear HSF1, and 1,437 were positive. Again, the positive cases had uniform HSF1 expression in nearly all of the cells. These positive cases were further subdivided according to the intensity of nuclear HSF1 staining: 882 demonstrated low-level staining, and 555 demonstrated high-level HSF1.
Interestingly, 40.5% of well-differentiated low-grade carcinomas were HSF1-negative and just 14.4% showed high nuclear HSF. In contrast, just 13.0% of poorly differentiated high-grade cancers were HSF1-negative, while 48.1% showed high HSF1 expression.
Levels of HSF1 also differed according to clinical parameters, the team continues. Those with high nuclear HSF1 expression were more likely to have been diagnosed at a more advanced clinical stage than HSF1-negative tumors, while high HSF1 expression was also more commonly observed in ER-negative, HER2-positive, and triple-negative cancers, “supporting an association between HSF1 expression and a more malignant phenotype,” they point out. Nuclear HSF1 was in addition detected in 84.5% of the ductal carcinoma in situ (DCIS) cases, with a similar frequency and level of expression as that observed in invasive cancers, although in the 200 DCIS cases examined there was no significant correlation between HSF1 expression and DCIS nuclear grade.
Looking more closely at the link between HSF1 expression and breast cancer survival, there was clear evidence that women with HSF1-positive tumors had worse survival than women with HSF1-negative tumors. In particular, a strong correlation was observed between HSF1-postive, ER-positive tumors and worse outcome. There was also overall evidence of a “dose-related” correlation, the team continues: survival decreased as HSF1 levels increased from none, to low, and then to high. This dose response wasn’t evident specifically among HER2-positive or triple-negative tumors, but was present in patients with ER-positive tumors.
To take into account all possible variables on the correlation between HSF1 levels and survival, the researchers assessed the relationship using several multivariate models. After adjusting for age, ER status, date of diagnosis, stage, grade, and treatment variables (radiotherapy, chemotherapy, and endocrine therapy), HSF1-positive tumors were associated with a 50% increase in breast cancer mortality: HSF1-low and HSF1-high tumors were associated with 45% and 62% increases in mortality, respectively. Similar results were seen in the ER-positive population, with HSF1-positivity correlating with an 86% increase in mortality. More specifically among the ER-positive tumors, HSF1-low and HSF1-high tumors were associated with 75% and 110% increases in mortality, respectively, relative to HSF1-negative, ER-positive tumors.
The same multivariate model in addition found a statistically significant association between HSF1 status and survival in patients with HER2-positive tumors, whereas the same multivariate model indicated there was no association between HSF1 status and survival among triple-negative patients. “The present study may simply have been underpowered to observe an effect of HSF1 in triple-negative patients because of the much smaller number of such cases in the NHS cohort and their molecular heterogeneity,” the authors suggest. “Alternatively, triple-negative tumors may have a decreased dependence on HSF1 because the underlying lesions do not require protection against diverse stresses or because other robust survival mechanisms are recruited.”
In a final series of experiments the researchers looked to see whether the associations between HSF1 protein level and breast cancer outcome could be detected by using HSF1 mRNA levels. mRNA expression profiling data aren’t available from tumors in the NHS, so the team instead used data from the publicly available van de Vijver cohort. The analysis results concurred with those form the IHC evaluation of tumors in the NHS cohort, and indicated that HSF1 mRNA levels were higher in ER-negative than in ER-positive cancers. Resulting Kaplan–Meier curves also indicated that women with HSF1-high, ER-positive tumors in the van de Vijver cohort had worse survival compared with women harboring HSF1-low, ER-positive tumors. This relationship wasn’t evident in the ER-negative tumor cohort. The team admits that additional work will be needed to more definitively conclude whether HSF1 acts as a prognostic factor in ER-negative tumors, however.
“In light of previous disappointing results with various individual HSPs as prognostic markers, the efficacy of HSF1, even as a single marker, in predicting the outcome of breast cancers is quite remarkable,” the authors conclude. “Our study suggests that HSF1 status might identify patients with ER-positive tumors who may benefit from more aggressive therapeutic management and others for whom less intervention may be warranted. In addition, HSF1 levels identify a large patient population in which targeting protein homeostasis and HSF1 function may be of therapeutic benefit…The findings support efforts to identify drugs that specifically target HSF1 function and ongoing work to develop inhibitors of HSP90 and other downstream pathways regulated by HSF1.”