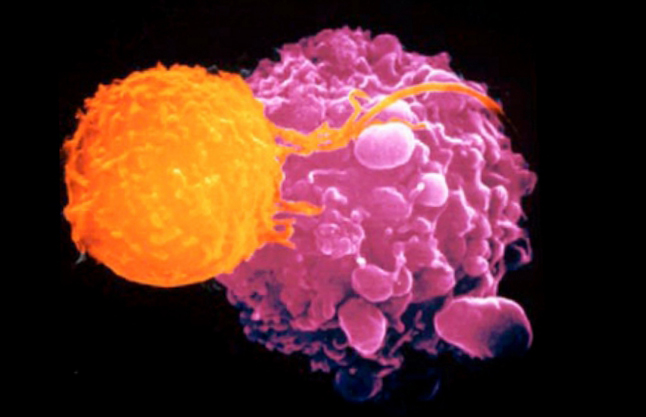
![Biopsies taken from patients who showed diverse responses to sequential checkpoint therapy were subjected to T-cell receptor sequencing and whole-genome sequencing. The sequencing results indicated that the effect of mutational load and burden of copy number loss on response was nonredundant, suggesting the potential utility of a combinatorial biomarker to optimize patient care with checkpoint blockade therapy. [University of New Mexico]](https://genengnews.com/wp-content/uploads/2018/08/T_cell2091215235-1.jpg)
Biopsies taken from patients who showed diverse responses to sequential checkpoint therapy were subjected to T-cell receptor sequencing and whole-genome sequencing. The sequencing results indicated that the effect of mutational load and burden of copy number loss on response was nonredundant, suggesting the potential utility of a combinatorial biomarker to optimize patient care with checkpoint blockade therapy. [University of New Mexico]
Immune checkpoint blockade, a therapy intended to boost the T-cell response to cancer, doesn’t always work, for reasons that aren’t always clear. If the reasons were better understood, this form of immunotherapy could become more effective. Ultimately, the reasons are genomic. For example, mutations can explain much of the variability in patient responses, but not all. Besides being guided by mutation information, say scientists based at the University of Texas MD Anderson Cancer Center, treatment plans may need to take account of copy number alterations, particularly those for tumor suppressor genes.
The MD Anderson team conducted whole-exome sequencing on tumor biopsies taken before, during, and after treatment of 56 patients. This work showed that outright loss of a variety of tumor-suppressing genes with influence on immune response leads to resistance of treatment with both cytotoxic T lymphocyte antigen (CTLA) and programmed death receptor-1 (PD1) inhibitors.
The team's research focuses on why these treatments help 20% to 30% of patients—with some complete responses that last for years—but don't work for others. Their findings indicate that analyzing loss of blocks of the genome could provide a new predictive indicator.
“There's no obvious correlation between mutations in cancer genes or other genes and immune response in these patients,” said Andrew Futreal, Ph.D., professor and chair of genomic medicine and co-leader of MD Anderson's Moon Shots Program. “There are, however, pretty strong genomic copy loss correlates of resistance to sequential checkpoint blockade that also pan out for single-agent treatment.”
Details of this work appeared March 1 in Science Translational Medicine, in an article entitled, “Integrated Molecular Analysis of Tumor Biopsies on Sequential CTLA-4 and PD-1 Blockade Reveals Markers of Response and Resistance.” The article describes how the MD Anderson scientists studied a cohort of melanoma patients treated with sequential checkpoint blockade against CTLA-4 followed by PD-1. This work led the scientists to identify immune markers of response and resistance.
“[We] performed deep molecular profiling including T cell receptor sequencing and whole-exome sequencing within the same cohort and demonstrated that a more clonal T cell repertoire was predictive of response to PD-1 but not CTLA-4 blockade,” wrote the authors of the Science Translational Medicine article. “Analysis of CNAs [copy number alterations] identified a higher burden of copy number loss in nonresponders to CTLA-4 and PD-1 blockade and found that it was associated with decreased expression of genes in immune-related pathways.”
“We found a higher burden of copy number loss correlated to response to immune checkpoint blockade and to lower immune scores, a measure of immune activation in the tumor's microenvironment,” noted Whijae Roh, a co-lead author of the current study and a graduate student in the MD Anderson UTHealth Graduate School of Biomedical Sciences. “We also found copy loss has an effect that is independent of mutational load in the tumors.”
Melanoma tumors with larger volumes of genetic alterations, called mutational load, provide more targets for the immune system to detect and are more susceptible to checkpoint blockade, although that measure is not conclusive alone. “Combining mutational load and copy number loss could improve prediction of patient response,” Wargo explained. When the team stratified patients in another dataset of patients by whether they had high or low copy loss or high or low mutational load, they found that 11 of 26 patients with high mutational load and low copy loss had a clinical benefit, while only 4 or 26 with low mutational load and high copy loss benefited from treatment.
In the trial, patients were treated first with the immune checkpoint inhibitor ipilimumab, which blocks a brake called CTLA-4 on T cells, the immune system's specialized warriors, freeing them to attack.
Patients whose melanoma did not react then went on to anti-PD1 treatment (nivolumab), which blocks a second checkpoint on T cells. Biopsies were taken, when feasible, before, during, and after treatment for molecular analysis to understand response and resistance.
To better understand the mechanisms at work, the team analyzed tumor genomes for recurrent copy loss among nine tumor biopsies from patients who did not respond to either drug and had high burden of copy number loss. They found repeated loss of blocks of chromosomes 6, 10, and 11, which harbor 13 known tumor-suppressing genes.
Analysis of a second cohort of patients confirmed the findings, with no recurrent tumor-suppressor loss found among any of the patients who had a clinical benefit or long-term survival after treatment.
The researchers also found a hint that treatment with ipilimumab, even if it fails, might prime the patient's immune system for successful anti-PD1 treatment.
The team analyzed the genetic variability of a region of the T-cell receptors, a feature of T cells that allows them to identify, attack, and remember an antigen target found on an abnormal cell or an invading microbe. They looked for evidence of T-cell “clonality,” an indicator of active T-cell response.
Among eight patients with longitudinal samples taken before treatment with both checkpoint types, all three who responded to anti-PD1 therapy had shown signs of T-cell activation after anti-CTLA treatment. Only one of the five nonresponders had similar indicators of T-cell clonality.
“That's evidence that anti-CTLA-4 in some cases primes T cells for the next step, anti-PD1 immunotherapy. It's well known that if you don't have T cells in the tumor, anti-PD1 won't do anything; it doesn't bring T cells into the tumor,” Dr. Futreal stated.
Overall, they found that T-cell clonality predicts response to PD1 blockade but not to CTLA-4 blockade.
“Developing an assay to predict response will take an integrated analysis, thinking about genomic signatures and pathways, to understand the patient when you start therapy and what happens as they begin to receive therapy,” Wargo remarked. “Changes from pretreatment to on-therapy activity will be important as well.”