A gene therapy being developed to treat Duchenne muscular dystrophy (DMD) successfully and safely stopped the severe muscle deterioration associated with the rare, genetic disease in both small and large animal models.
The study, “Non-immunogenic utrophin gene therapy for the treatment of muscular dystrophy animal models” published in Nature Medicine, found that a gene therapy successfully stopped the severe muscle deterioration associated with the disease—without triggering immune responses known to hinder previous therapeutic approaches.
The findings, conducted in mice and two different DMD dog models, may refocus the field toward the use of a utrophin-based gene therapy approach as the pathway to a patient cure for DMD.
Found mostly in boys, DMD is caused by mutations in a sex-linked gene that stops the production of the protein dystrophin. Without it, muscles progressively deteriorate and weaken starting at a very young age and only worsen from there. Most patients aren’t able to walk by age 12 and die of heart or respiratory failure by the time they reach their 30s, though respirators have helped some live longer.
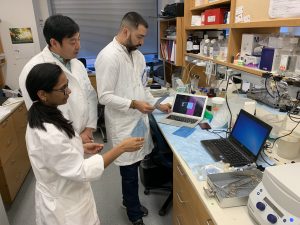
With their modified gene therapy approach, a multidisciplinary team from the Perelman School of Medicine at the University of Pennsylvania (UPenn) engineered adeno-associated virus (AAV) vectors to deliver a “substitute” protein for dystrophin in small and large animal DMD models to keep the muscles intact. The synthetic substitute, based on a naturally occurring protein called utrophin, proved to be an effective and safe alternative, as it protected muscle in mice and dogs with naturally occurring DMD-like mutations, including a large deletion that closely mirrors the large dystrophin deletions found in humans.
“For the first time, we’ve shown how a carefully constructed version of a dystrophin-related protein can safely prevent the breakdown of muscle and maintain its function over time in the most informative animal models. This discovery has important implications for gene therapy and how we work toward safe and effective treatments for muscular dystrophy,” said senior author Hansell Stedman, MD, an associate professor of surgery at UPenn. “With these results, we have a strong rationale to move this forward into human clinical trials.”
In an accompanying News and Views article, titled “Surrogate gene therapy for muscular dystrophy”, Dame Kay Davies, PhD, professor of anatomy at the University of Oxford and Jeffrey S. Chamberlain, PhD, professor of neurology at the University of Washington, write that “although current gene therapy trials for DMD are showing encouraging results, a rigorous test of dystrophin immunity has not been performed, and the availability of μ-Utro vectors provides an important alternative approach to treating this devastating human genetic disorder.”
Restoring levels of dystrophin with gene therapy and other techniques have been under scrutiny due to the immune system’s adverse reaction to additions it deems foreign. DMD patients have little to none of this protein, so their bodies can attack well-intentioned direct replacement proteins because they are seen as foreign. However, because dystrophin’s distant cousin utrophin is expressed in other places in the body, it was thought that the immune system wouldn’t view it as a threat.
The UPenn team showed this to be true in rigorous, randomized mouse and dog studies. Delivering a single-dose treatment of synthetic utrophin with the AAV vector to newborn mice showed distribution of the protein throughout the body, no signs of toxicity, and complete suppression of all signs of DMD, compared to untreated mice. The mice also sustained expression of utrophin in skeletal and cardiac muscles throughout that time, and physical tests in the mice supported the sustained muscle function.
The team further investigated utrophin by administering it to dogs four to seven days of age in a randomized study. Six weeks after receiving a dose, the researchers observed a robust expression of utrophin and a four-fold increase in weight compared to previously reported weight loss and body-wide inflammation, suggesting induced “auto”-immunity in dogs who received human dystrophin. The researchers also observed a significantly reduced level of muscle damage in the treated dogs.
Researchers compared utrophin-treated limbs with dystrophin-treated limbs, and after four weeks, observed stark differences. Muscle biopsies revealed persistent expression of utrophin and suppression of ongoing muscle damage, but only sparse amounts of dystrophin in dying cells in the other limb. The immune responses also varied greatly between the limbs.
“Under the microscope it looked like a hand grenade had gone off in the limbs with dystrophin,” Stedman said. “The experiments showed that the immune response to dystrophin was 100 to 1,000 times stronger than it was to utrophin.”
Treated dogs also had nearly complete prevention of muscle degeneration and regeneration in their jaw closing (biting) muscles. These muscles, by virtue of their extreme power, are among the first to deteriorate in untreated dystrophic dogs.
This is the first large animal study to show utrophin’s effectiveness as well as its non-immunogenic response. Taken together, the researchers said, these findings may refocus the field toward the use of a functionally optimized, safe utrophin-based gene therapy approach as the pathway to a potential cure for Duchenne muscular dystrophy.

![Spark Therapeutics saw its share price tumble about 30% in early-morning trading after it reported mixed preliminary data this morning from a Phase I/II trial of its hemophilia A gene therapy candidate SPK-8001. [Source: wildpixel/Getty Images] Spark Therapeutics saw its share price tumble about 30% in early-morning trading after it reported mixed preliminary data this morning from a Phase I/II trial of its hemophilia A gene therapy candidate SPK-8001. [Source: wildpixel/Getty Images]](https://www.genengnews.com/wp-content/uploads/2018/08/Dec7_2017_Getty_487489316_GeneTherapy_60019871441892139879144.jpg)




