October 1, 2011 (Vol. 31, No. 17)
Rita Colwell, Ph.D.
Bringing Modern Technology to Bear on Potential Threats
Less than one-third of the world population has access to safe drinking water, with the result that death rates for children under the age of five are 200 or more per 1,000. In developed countries nearly all have access to safe drinking water and the death rates of children from waterborne diseases are significantly lower.
Cholera is a waterborne disease with a very long history; it is currently considered by developed countries to be introduced from elsewhere, despite significant evidence that Vibrio cholerae, the causative agent of cholera, inhabits rivers, ponds, estuaries, and coastal waters globally, even in Iceland, where the disease has never been recorded.
Historically, cholera epidemiology traces to a physician, Sir John Snow, who published reports of his studies of the cholera epidemics of 1849 and 1854 in London. Snow traced the source of the London epidemics of cholera to water drawn from the Broad Street well. A now famous map was prepared by Snow, who marked on the map those houses on the streets in which deaths from cholera had occurred, providing evidence for his conclusion that water pumped from the Broad Street well was the source of the disease.

Rita Colwell, Ph.D.
Yet, 20 years passed before Snow’s correlation was accepted, namely that contaminated water was the source of the London cholera epidemics.
Cholera is more than an unfortunate historical bookmark of history. Data on cholera incidence worldwide, compiled by the World Health Organization, shows that this disease affects millions even today. Writ large are the tragedies of Zimbabwe and Haiti. Cholera cases reported in Zimbabwe in 2007 numbered approximately less than 100 and one year later, by 2008, breakdown of the water purification and distribution system in that country resulted in a massive epidemic of more than 110,000 cases and ca. 4,000 deaths.
The epidemic in Zimbabwe continues today, but even more tragic is the cholera outbreak in Haiti. Cholera followed an earthquake, hurricane, and flooding, creating untold misery for refugees from these natural events.
Discoveries made more than 20 years ago at the University of Maryland showed the cholera vibrio to be naturally present in the environment and, under conditions adverse to growth, to enter into a dormant state. For example, when exposed to temperatures less than 15°C, V. cholerae cannot be cultured under routine laboratory conditions and is detectable only by molecular methods, such as staining with a fluorescent antibody or by genetic analysis.
The bacterium under such conditions can remain viable for months and even though not culturable, is transmissible and able to cause disease, as was shown in both animal experiments and human volunteer studies. With a fluorescent antibody or gene probe, the cholera bacterium can be detected in water samples when it cannot be cultured. The accepted dogma had been that cholera could be transmitted only person to person, but that assumption was proven wrong when the bacterium was found to be present naturally in the aquatic environment, using tools of modern microbiology.
Studies of V. cholerae in bays and estuaries in the U.S., Asia, and Africa showed this microorganism to be a component of the natural flora of zooplankton, predominantly copepods, the microscopic shrimp-like animals. Since a single copepod can carry 10,000 or more cholera bacteria on its surfaces and in its gut, when the zooplankton population increases significantly during its spring and fall “blooms,” an infectious dose of the cholera bacteria can be ingested by those who drink untreated water.
In 1991–1992, a massive epidemic of cholera occurred in Latin America years after the disease had apparently been absent from South American countries. Since the “home” of cholera historically was considered to be South Asia, the Latin American epidemic caught public health authorities by surprise. In the U.S. and Western Europe, cholera has been controlled since the early twentieth century by providing safe drinking water.
Initiation of the Latin American cholera epidemic has since been linked to climate, notably the El Niño of 1991–1992. The relationship in aquatic systems between water temperature, salinity, and plankton populations, with cholera has been explored extensively.
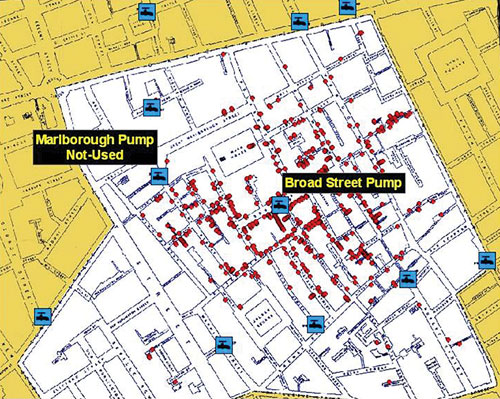
Sir John Snow was able to trace the source of the London cholera epidemics of 1849 and 1854 to one specific well. Twenty years passed before his assertion that contaminated water was the source of the cholera epidemics was accepted.
Benefits of Filtering
Mathematical models, employing physical-chemical parameters, including salinity, nutrient concentrations, pH, water temperature, presence of plankton, etc., have been developed showing climate and cholera correlation. Poor sanitation and lack of safe drinking water, of course, exacerbate the disease once it is initiated. Thus, environmental parameters associated with cholera can be monitored using satellite sensors and those parameters, which are monitored by satellite, such as sea surface temperature, sea surface (tidal) height, and chlorophyll, provide data for the models.
The results have provided good estimates of the number of cholera cases in Bangladesh, India, and Africa. Based on these findings, the hypothesis was developed that, since plankton carry cholera bacteria, if a simple filter is properly employed when collecting drinking water from untreated sources, such as ponds and rivers, the incidence of cholera could be reduced.
A study was conducted and several materials were tested. A field study carried out in Bangladesh, comprising 150,000 inhabitants in 50 villages, was executed over a three-year period. Bangladeshi village women trained in the use of simple cloth filters to collect water, with cooperation by village women, reinforced filtration as a method to remove particulate matter, notably plankton, since the cholera bacteria attached to the plankton would therefore also be removed. Incidence of cholera in families practicing simple filtration was reduced by approximately 50%.
A follow-up study conducted five years after the initial study ended showed filtration was sustainable, i.e., the village women continued the practice of simple filtration. Hence, it proved both sustainable and effective.
In 2000, the first genome of the cholera vibrio was sequenced. Since then, the DNAs of many additional strains of V. cholerae have been sequenced. The cholera isolates included historical strains, such as V. cholerae isolated in 1910 and geographically diverse isolates from Africa, India, the Sudan, etc. What was discovered was that the genomic sequence of these strains shows detectable variation. That is, there is a significant genetic exchange among V. cholerae, i.e., sets of genes found in V. cholerae transfer from strain to strain within V. cholerae populations. The evolution of V. cholerae was, thus, tracked by following gain and loss of sets of genes coding for pathogenic properties and serotype.
The studies conclusively showed that genes coding for serotype are laterally transferred. The cholera bacterium, in effect, undergoes genetic “drift and shift,” becoming a moving target for public health workers.
In summary, these studies of cholera in Bangladesh, India, Africa, and the U.S. have provided a model for understanding the emergence of this disease from the natural environment globally. Cholera is an excellent example of an environmental bacterium that has the potential to cause massive epidemics in human populations worldwide. It is an excellent example of how we must understand our environment and the living system it comprises.
The message, therefore, is dual: safe water is a critical necessity for humankind and the complexity of our biological world must be more fully understood for its beneficial gifts and its potential threats.
Rita Colwell, Ph.D. ([email protected]), is Distinguished University Professor at both the University of Maryland, College Park and Johns Hopkins University Bloomberg School of Public Health.







