All tissues are not equally sensitive to radiation. It has long been recognized that the well-known tumor suppressor protein and transcription factor p53 is linked to the degree of a tissue’s sensitivity to radiation. Yet how p53 regulates vulnerability to radiation has been elusive so far.
In an article titled “p53 dynamics vary between tissues and are linked with radiation sensitivity,” published in Nature Communications, scientists at the Blavatnik Institute at Harvard Medical School, Massachusetts General Hospital, and the Novartis Institutes for BioMedical Research clarify that it is not the abundance of p53 protein in a tissue’s that correlates with the tissues’ sensitivity to radiation but the dynamics of p53 signaling following radiation.
The new study finds radiosensitive tissues show persistent p53 signaling while more resistant tissues show brief p53 activation, after being exposed to radiation. The study demonstrates that cell survival after radiation exposure depends on behavior of p53 over time. In vulnerable tissues, p53 levels go up and remain high, leading to cell death while in tissues that survive radiation damage, p53 levels swing up and down.
“Dynamics matter. How things change over time matters,” says Galit Lahav, PhD, the Novartis Professor of Systems Biology at Harvard Medical School and co-corresponding author on the study. “Our ability to understand biology is limited when we only look at snapshots. By seeing how things evolve temporally, we gain much richer information that can be critical for dissecting diseases and creating new therapies.”
The study reports certain types of tumors in mice are more vulnerable to radiation after administered a drug that prevents p53 levels from going down or pulsing. This dual treatment is more effective than radiation or the drug alone, suggesting new strategies to improve combination therapies for cancer.
“We were able to connect differences in temporal p53 expression with radiation response, and these insights allowed us to ‘coax’ radioresistant tumors into more radiosensitive ones,” says Ralph Weissleder, PhD, the Thrall Family Professor of Radiology and HMS professor of systems biology at Mass General and co-corresponding author on the study. “This is an incredibly exciting study showing that basic science done in rigorous quantitative fashion can lead to new important clinical discoveries.”
Cellular suicide in the face of irreparable genomic damage to protect the organism, is the role of p53. Previous studies from the group have revealed the dynamic behavior of p53 over time and its role in cancer drug efficacy, cell fate, and more.
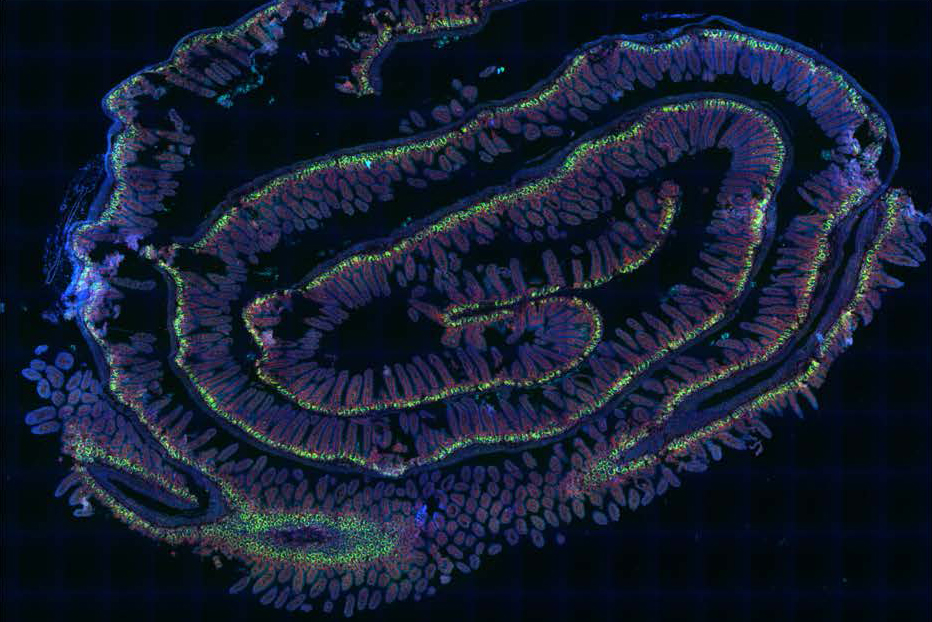
In the current study the team looks at tissues in mice that have different sensitivities to ionizing radiation but no difference in p53 levels–the spleen and thymus, which are highly vulnerable, and compare these to the large and small intestines, which are more radioresistant.
In the absence of stress, cells express little or no p53. After radiation exposure, all four tissues express high levels of p53 and other markers of DNA and cellular damage. Quantitative imaging analyses shows p53 in the intestines peaks and then declines a few hours after irradiation whereas in the radiosensitive spleen and thymus p53 levels remain high.
The team uses an experimental anti-cancer drug to inhibit MDM2, a protein that degrades p53. Blocking MDM2 activity after radiation exposure, forces p53 levels to remain high in cells where it would otherwise go down. In the intestine, which is normally radioresistent, the drug reduces cell survival.
To address whether regulating p53 dynamics could increase tumor vulnerability, particularly those that become resistant to radiation, the researchers focus on human colon cancer cell lines with intact p53.
In a model system where human colon cancer tumors were transplanted into mice, radiation followed by MDM2 inhibitor administration showed significant tumor shrinkage and remained smaller even 6 weeks post-treatment, compared to tumors treated with the drug or radiation alone.
“By irradiating first, we force the cancer cells to activate p53, and by adding MDM2 inhibitor on top of that, we can keep p53 active longer,” says Lahav. “This combination has a much stronger effect than either alone.”
Biological pathways that lead to differences in p53 dynamics remain a question for future study. Further studies will also help determine how best to combine and time therapies that exploit p53 dynamics to improve cancer treatment.
“For a lab studying p53, cancer is always a major motivation. Our goal is to acquire knowledge to help develop better and more efficient therapies,” says Lahav. “Understanding how p53 behaves over time in different conditions is a critical piece of the puzzle.”