Celiac disease (CD) is an autoimmune disorder that causes gastrointestinal symptoms and damage to the lining of the small intestine upon ingestion of gluten—a protein found in grains such as wheat, barley and rye. The cause is not well understood and there are no available therapeutics. For these reasons, more sophisticated research is paramount for the estimated 1% of people who have CD.
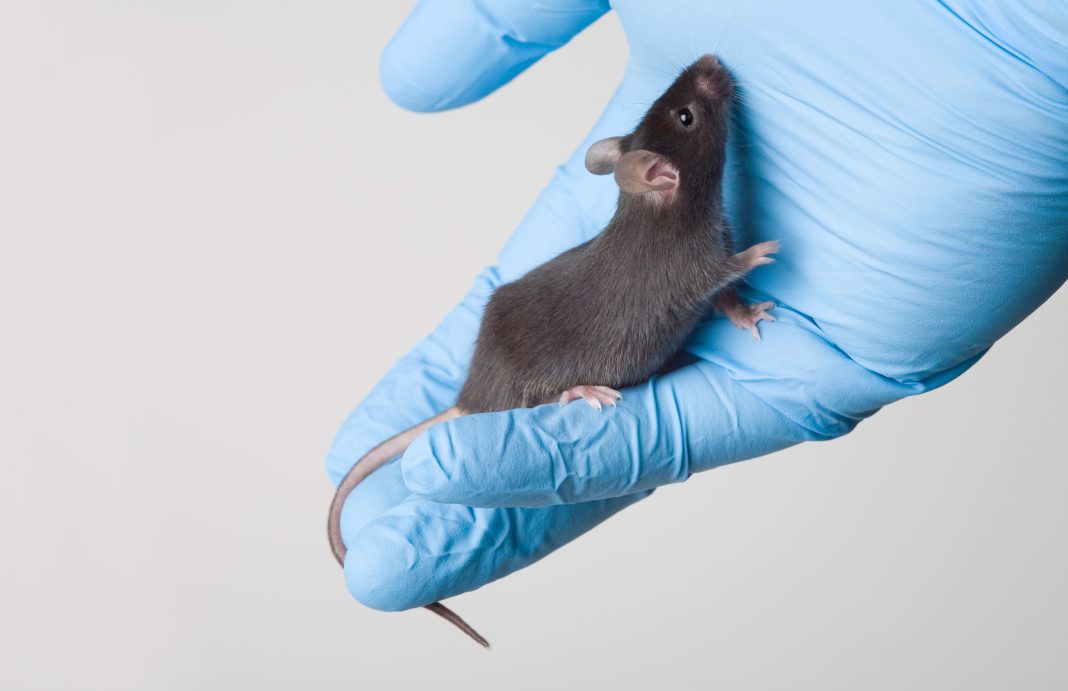
Researchers at the University of Chicago have announced a huge leap forward, through the development of the first truly accurate mouse model of CD. The animals have the same genetic and immune system characteristics as humans who develop CD, and will provide a vital research tool for developing and testing new treatments for the disease.
The work is published in Nature in the study, “IL-15, gluten and HLA-DQ8 drive tissue destruction in coeliac disease.”
“Based on our understanding of the human disease, we were able to retro-engineer a mouse model of celiac disease,” said Bana Jabri, MD, PhD, director of Research at the University of Chicago Medicine Celiac Disease Center and senior author. “It’s the first model where the mouse develops damage to the small intestine just by eating gluten, which can later reverse itself on a gluten-free diet.”
The only effective treatment for CD is to maintain a gluten-free diet, which can be challenging and expensive. Accidental ingestion of gluten through unknown ingredients in processed food, or cross-contamination from foods containing gluten that are prepared nearby or with the same cooking equipment, is a constant concern.
Even while maintaining a strict gluten-free diet, 40% of CD patients still show signs of inflammation and villous atrophy, or damage to the villi, the small, finger-like protrusions in the small intestine that help absorb nutrients. Therefore, treatments that can reverse or prevent the disease are greatly needed to improve quality of life for people with CD.
A complex interplay of contributing factors
Scientists do not know the exact cause of CD, but researchers have identified several genetic, immune system, and environmental components that work together to trigger the disease.
The inflammatory enteropathy, caused by exposure to dietary gluten, occurs in a subset of genetically susceptible individuals who express either the HLA-DQ8 or HLA-DQ2 haplotype. However, possessing one these variants is not sufficient to develop the disease alone.
Based on studies in CD patients, Jabri and her colleagues have proposed that signs of tissue distress associated with high levels of an inflammatory protein called IL-15 in the lining of the small intestine were required to cause villous atrophy, the hallmark of the disease.
In the paper, the team describes a mouse model that “reproduces the overexpression of interleukin-15 (IL-15) in the gut epithelium and lamina propria that is characteristic of active coeliac disease, expresses the predisposing HLA-DQ8 molecule, and develops villous atrophy after ingestion of gluten.”
Certain environmental factors may come into play as well. In 2017, for example, Jabri and her team discovered that a common virus can cause changes to the immune system that set the stage for CD. All of these factors work together to trigger an autoimmune response when someone ingests gluten that causes villous atrophy.
For more than 20 years, researchers have attempted to develop a mouse model for CD that reflects these conditions. However, none of these models resulted in mice with one of the HLA gene variants that also developed villous atrophy in response to gluten.
“In celiac, the main feature of disease is tissue destruction of the small intestinal lining,” said Valérie Abadie, PhD, a research assistant professor at UChicago and lead author of the study. “This new HLA-DQ8 mouse model is unique because it’s the only one that actually develops villous atrophy when the animal does eat gluten. In addition, once the mice are placed on a gluten-free diet, their small intestine can recover and heal, just as in humans with celiac disease.”
Jabri said that all of these elements must be present in a research model to truly represent the conditions that cause disease in humans. “It’s like a puzzle where different pieces need to come together for everything to fall into place,” Jabri said. “If you have a model where only one piece of the puzzle causes the disease because it’s in a laboratory setting, then you cannot test how to block or interfere with the other components. You need to have a setup where you have the entire complex interplay that takes place for the development of celiac disease.”
The new mouse model provides a vital tool for developing new treatments to reverse CD once it has developed or prevent it from developing in people at risk for the disease. Researchers will be able to identify new targets for drugs and then test them in a model that faithfully represents the condition in humans.
“This wouldn’t be possible without first conducting human studies to understand the nature of the disease,” Jabri said. “Now, using the mouse model, we can interrogate more and apply what we learned back into the human system. The integration of those two approaches is very important.”